Is Late-Onset Crohn's Different? Understanding the Risks
"New research sheds light on how Crohn's disease manifests differently depending on when it starts, influencing potential complications and treatment strategies."
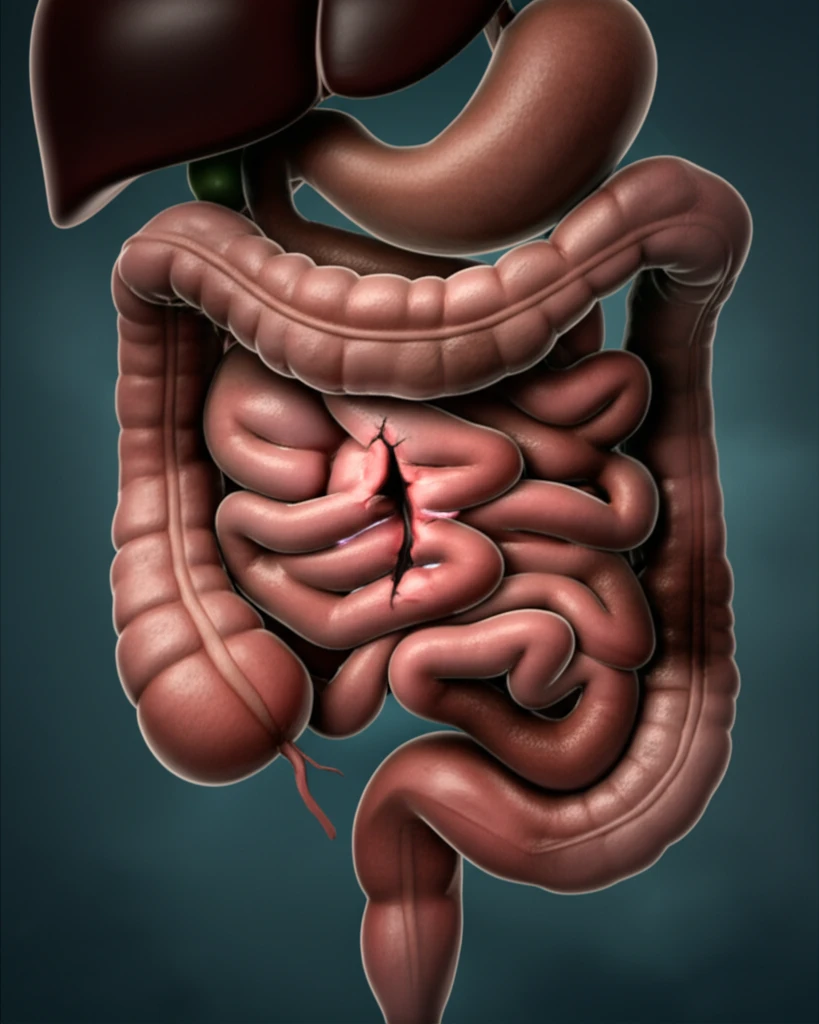
Crohn's disease, a chronic inflammatory condition of the digestive tract, doesn't always manifest in the same way. Research increasingly suggests that the age at which Crohn's disease begins can significantly influence its characteristics and potential complications. This article explores the key differences between early-onset and late-onset Crohn's disease, drawing on recent research to highlight the unique risks associated with the latter.
Understanding these differences is crucial for both patients and healthcare providers. By recognizing the distinct patterns of late-onset Crohn's, medical professionals can tailor diagnostic and treatment approaches to optimize patient outcomes. For individuals experiencing symptoms later in life, awareness of these nuances can empower them to seek timely and appropriate care.
This article will delve into a study comparing the clinical features of early-onset versus late-onset Crohn's disease, focusing specifically on the risk of intestinal perforation and perianal fistula. We will break down the findings in an accessible way, providing clear insights into how age of onset impacts the disease course and management strategies.
Late-Onset Crohn's: Higher Risk of Intestinal Perforation
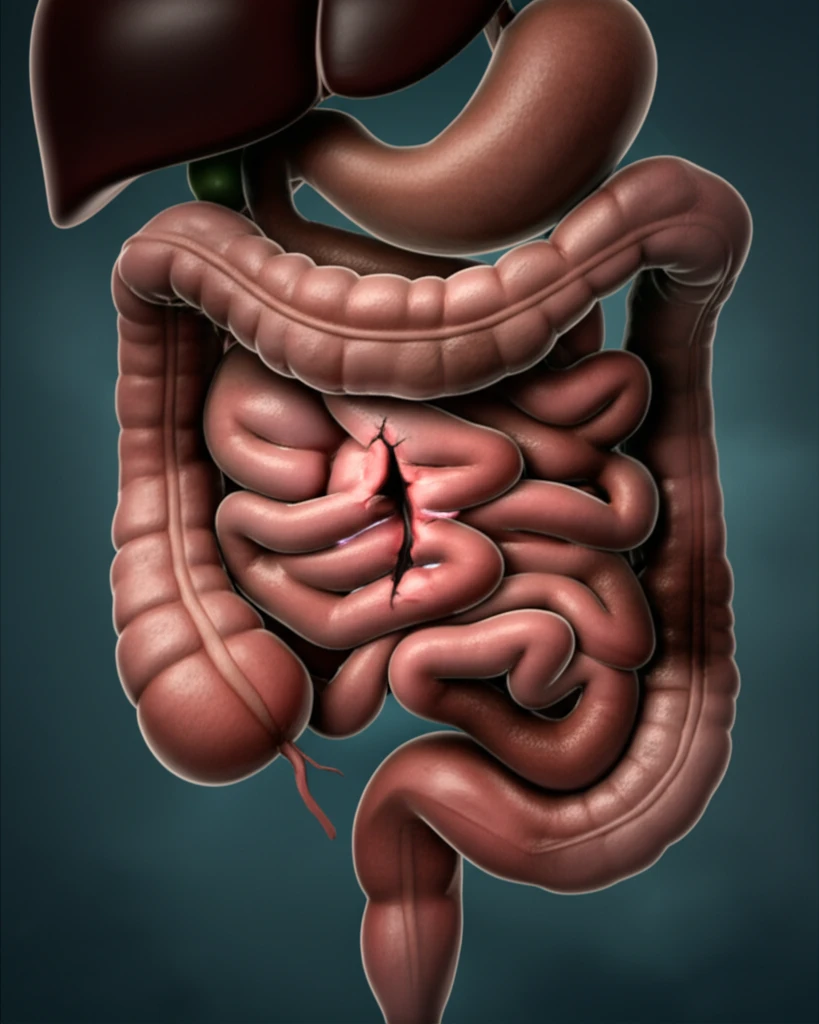
A recent study investigated the differences between early-onset (diagnosis before age 40) and late-onset (diagnosis at age 40 or later) Crohn's disease, utilizing data from the CONNECT cohort. The research revealed a significant trend: patients with late-onset Crohn's disease face a higher risk of intestinal perforation compared to those diagnosed earlier in life.
- Increased Surgical Intervention: Late-onset Crohn's patients underwent abdominal surgery more frequently (33.0%) than their early-onset counterparts (25.0%).
- Elevated Intestinal Perforation Risk: The multivariable analysis showed that late-onset Crohn's disease had an odds ratio of 3.090 (95% CI: 1.228-7.772, p=0.017) for intestinal perforation. This indicates a statistically significant higher risk.
Key Takeaways and Implications
The research highlights a crucial distinction in Crohn's disease presentation based on age of onset. Late-onset Crohn's disease appears to be associated with a higher risk of intestinal perforation, necessitating careful monitoring and potentially more aggressive management strategies.
For individuals diagnosed with Crohn's disease later in life, it's essential to be aware of this increased risk and to discuss preventive measures and early warning signs with their healthcare provider. Prompt attention to symptoms and proactive management can significantly improve outcomes.
Further research is warranted to explore the underlying causes of these differences and to develop targeted therapies that address the specific challenges of late-onset Crohn's disease. Understanding the nuances of Crohn's presentation across different age groups is key to optimizing patient care and improving long-term outcomes.
