Interrupted Aortic Arch Repair: A Lifelong Journey
"Discover the long-term outlook for patients undergoing interrupted aortic arch repair and how medical advancements are paving the way for improved outcomes."
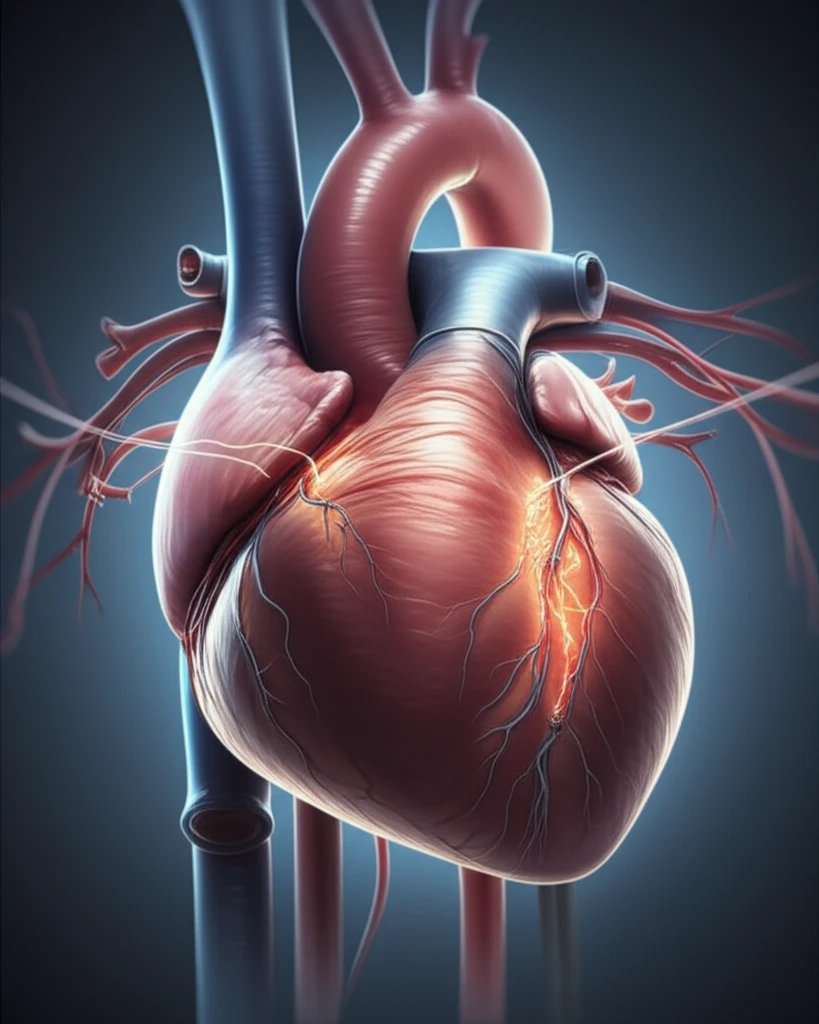
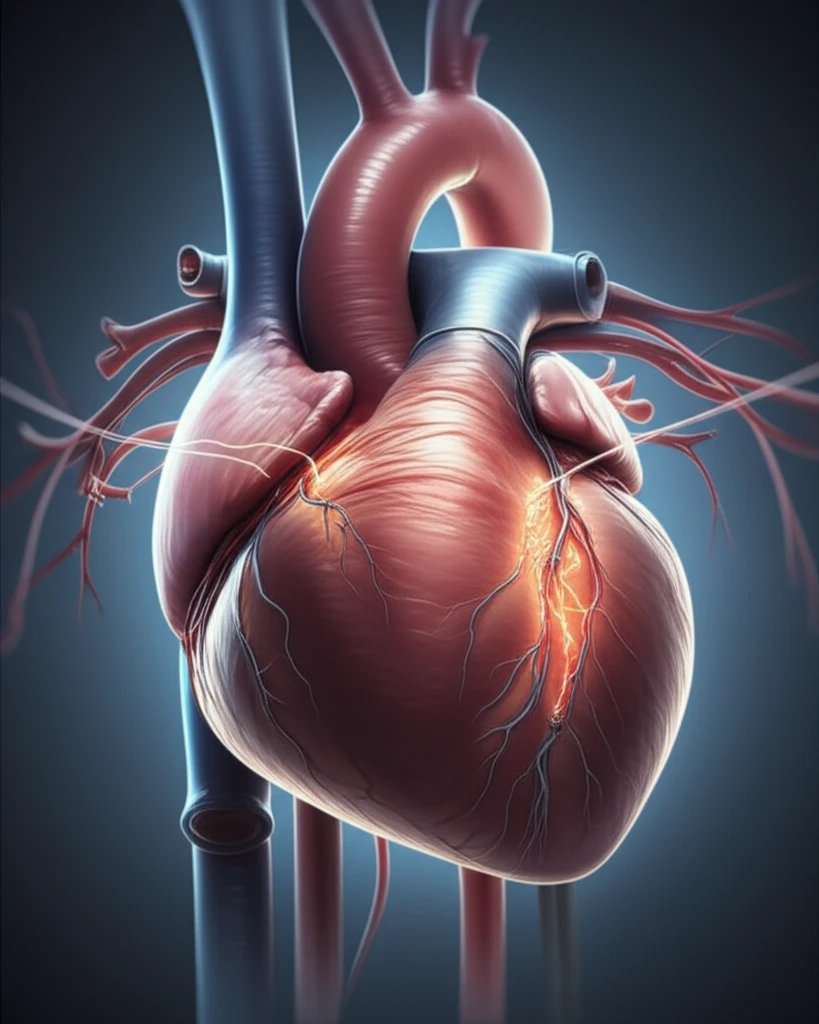
Interrupted aortic arch (IAA) is a rare congenital heart defect where the aorta, the body's main artery, isn't fully formed. This condition disrupts blood flow, posing significant risks to infants. While surgical repair techniques have advanced, understanding the long-term outcomes remains crucial for optimizing patient care.
A recent study published in The Annals of Thoracic Surgery delves into the outcomes of IAA repair using direct anastomosis and homograft augmentation patch. This technique involves connecting the separated segments of the aorta and reinforcing the connection with a patch. The study offers valuable insights into the effectiveness and durability of this approach over an extended period.
This article breaks down the study's findings, translating complex medical information into accessible language. We'll explore the surgical methods, long-term results, and factors influencing patient outcomes, offering a comprehensive overview for anyone interested in understanding this complex condition.
Decades of Data: Understanding the IAA Repair Journey
Researchers conducted a single-center study, gathering data from 1988 to 2015 on 120 patients who underwent IAA repair. The patients were categorized into four groups based on the presence of other heart defects:
- IAA with ventricular septal defect (VSD)
- IAA with Norwood/Damus-Kaye-Stansel (DKS) procedure (typically for hypoplastic left heart syndrome)
- IAA with truncus arteriosus
- Miscellaneous group (including other complex heart defects)
Looking Ahead: Optimism and Ongoing Research
This study confirms that direct anastomosis with patch augmentation offers a reliable approach for IAA repair, providing good long-term arch patency across various anatomical types. The findings highlight the importance of weight at surgery as a critical factor influencing survival rates. While surgical techniques have improved significantly, ongoing monitoring and potential re-interventions remain a consideration for these patients.
The findings suggest that focusing on optimizing the patient's condition before surgery, particularly ensuring adequate weight gain, could lead to even better outcomes. Further research is needed to explore strategies for minimizing the need for re-interventions and addressing potential long-term complications.
Ultimately, this study provides valuable data for cardiologists, surgeons, and families of children with IAA, offering a clearer picture of the long-term journey and the ongoing efforts to improve the lives of these patients.
