ICU Dilemmas: Finding Dignity in the Chamber of Torture
"Navigating end-of-life care and ethical decisions in the intensive care unit."
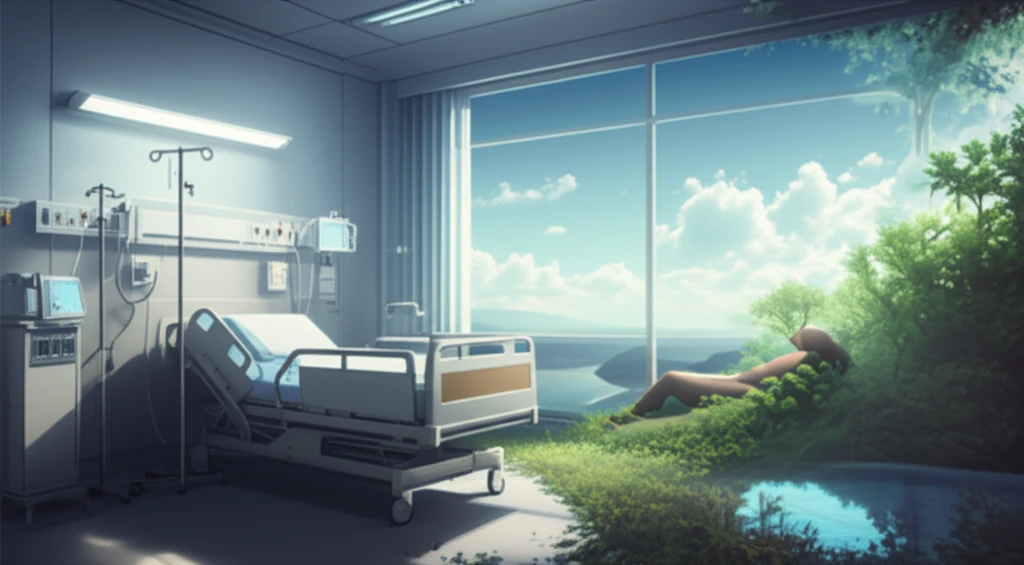
In the high-stakes environment of the Intensive Care Unit (ICU), patients often face a reality far removed from the promise of a quick return to health. Contrary to the image of miraculous recoveries often portrayed in television dramas, many ICU patients are battling chronic or incurable diseases in their final stages of life.
The ICU environment, filled with ventilators, dialysis machines, and a constant stream of medications, can become a place where the focus shifts from healing to merely prolonging existence. Families often witness their loved ones enduring invasive procedures and discomfort, raising difficult questions about the true value of aggressive medical intervention.
This article delves into the ethical and emotional complexities of end-of-life care in the ICU, drawing from a study published in the Journal of Palliative Care & Medicine. It explores how palliative medicine and bioethics can provide a more compassionate and dignified approach to death and dying, offering relief for both patients and their families.
The Ethical Minefield of Modern Medicine
Modern medicine possesses the remarkable ability to sustain life, but this power often leads to ethical dilemmas, particularly in the ICU. The mandate to "do everything" can result in patients suffering through futile treatments, extending life without improving its quality. The fear of facing death, coupled with a reluctance to disappoint patients and families, can drive medical professionals to pursue aggressive interventions even when the prognosis is grim.
- The Illusion of Control: Technology can defy natural selection, prolonging life in situations where the body is unable to recover.
- The Fear of Death: Doctors may be reluctant to acknowledge the inevitability of death, leading to the continuation of futile treatments.
- Ethical Dilemmas: Families grapple with questions about the will of God, the definition of suicide, and the responsibility to make decisions when their loved ones can no longer speak for themselves.
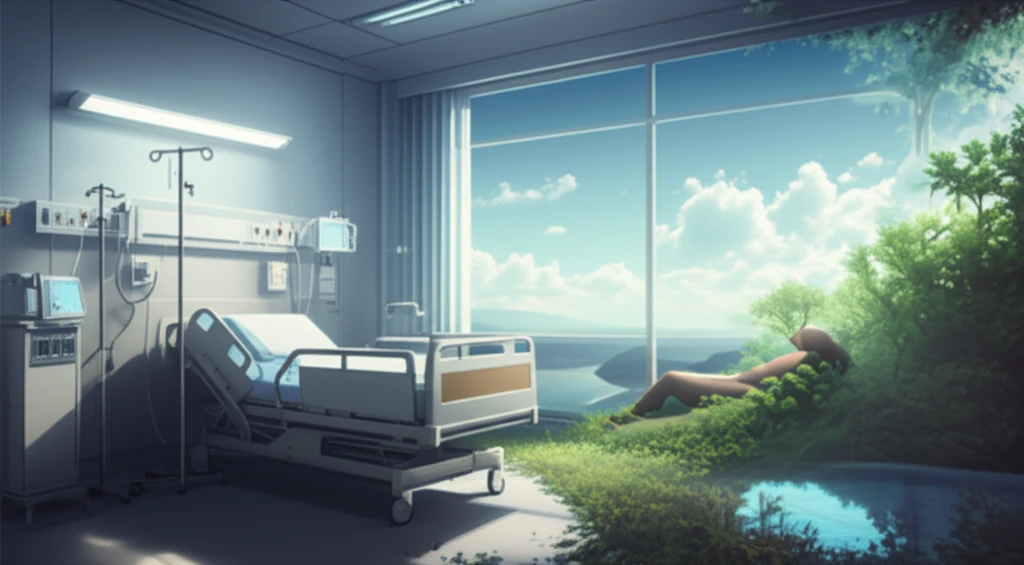
Finding a More Compassionate Path
The key to improving end-of-life care in the ICU lies in shifting the focus from merely prolonging life to prioritizing quality of life. This requires open and honest communication between physicians, patients, and families, as well as a willingness to consider alternative approaches, such as palliative care.
Both physicians and families need to understand that there is a moral, ethical, and legal right to allow natural death and avoid unnecessary suffering. Treatment goals at the end of life should focus on providing emotional and medical support while maintaining quality of life. Making the final outcome a more pleasant and less painful experience for families and most importantly, the patient.
By embracing bioethics and palliative medicine, we can create a more compassionate and dignified experience for those facing the end of life in the ICU. Further research, like the study of AYAs with cancer, is crucial to understanding the unique needs of specific populations and informing health policy guidelines to support them through this difficult stage.
