HIFU for Liver Cancer: A New Hope or a Risky Procedure?
"Exploring the benefits and potential complications of High-Intensity Focused Ultrasound (HIFU) in treating advanced liver cancer"
Liver cancer, or hepatocellular carcinoma (HCC), ranks among the most prevalent and deadly cancers globally. Often, it's diagnosed at an advanced stage when the patient's liver function is already compromised, leaving many without the option of surgery. For these individuals, treatments like transcatheter arterial chemoembolization (TACE), targeted drugs, and radiofrequency ablation (RFA) offer some hope, but they come with their own limitations, like being unsuitable based on the size or location of the tumor.
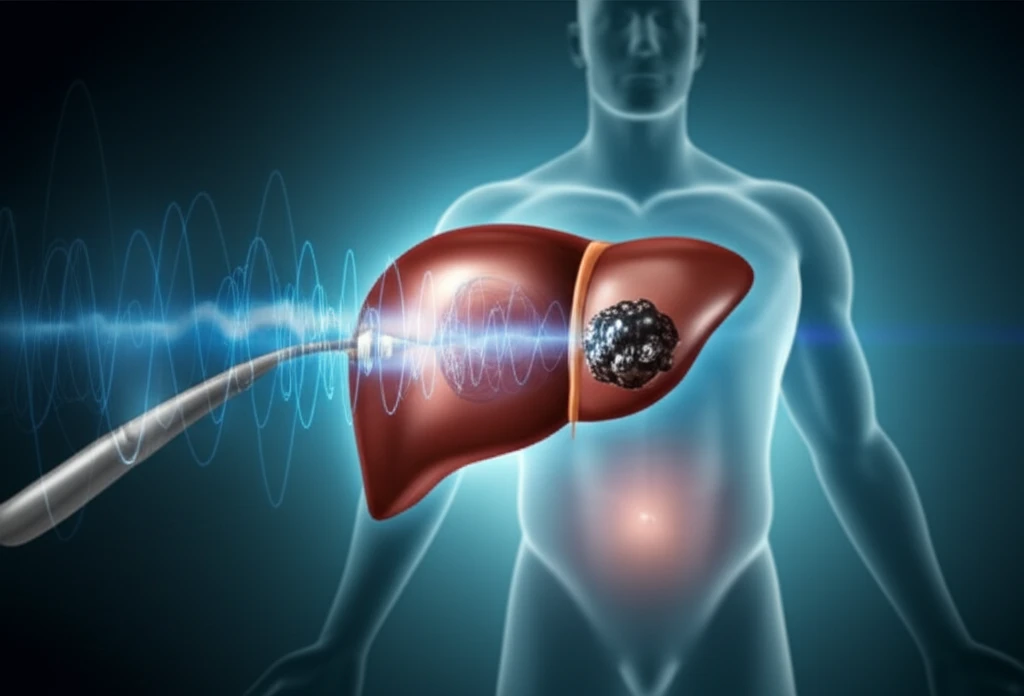
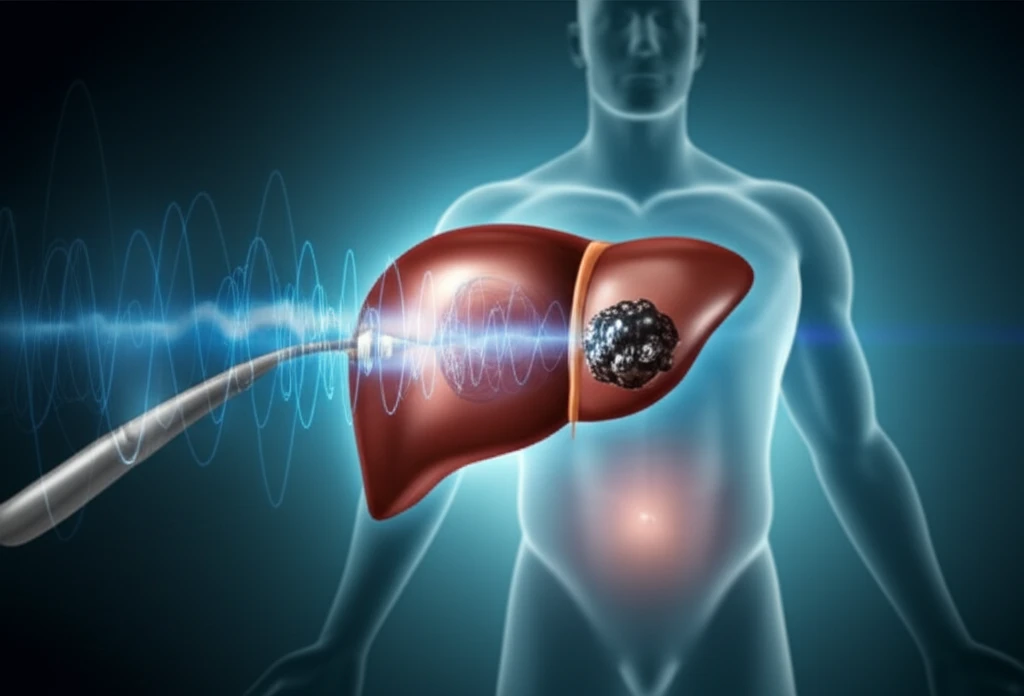
High-Intensity Focused Ultrasound (HIFU) has emerged as a promising alternative. HIFU is a localized thermal ablation therapy known for being minimally invasive, promoting quicker recovery, and enhancing the body’s immune response against the tumor. It allows for precise, three-dimensional treatment of solid tumors, making it a valuable option for those with advanced HCC.
A recent case study sheds light on the potential of HIFU in treating unresectable, massive HCC. While the treatment demonstrated effectiveness, it also led to an unusual complication: a chest wall hernia. This article explores the details of this case, offering insights into the benefits and risks associated with HIFU therapy for liver cancer.
The Case Study: Promising Results with an Unexpected Twist
In September 2010, a 57-year-old male was admitted with complaints of abdominal distension. His medical history included a 30-year battle with hepatitis B, which had gone largely untreated. Scans revealed a significant mass in the right lobe of his liver, suspected to be HCC, along with intrahepatic metastasis, cirrhosis, splenomegaly, and portal hypertension. His alpha-fetoprotein (AFP) levels, a marker for liver cancer, were alarmingly high at 3,200 ng/ml.
- Tumor Regression: Follow-up scans showed a significant reduction in tumor size.
- Pain Relief: The patient experienced noticeable pain reduction.
- AFP Levels: The levels of alpha-fetoprotein, a marker for liver cancer, decreased.
- Chest Wall Hernia: A previously unreported complication emerged.
HIFU: Weighing the Benefits and Risks
HIFU offers a valuable alternative for patients with advanced HCC who are not candidates for surgery, TACE, RFA, or targeted drug therapies. While this case study highlights the potential for effective tumor control and improved survival, it also brings to light the importance of understanding and managing potential complications, such as chest wall hernia. As with any medical procedure, a thorough evaluation of the patient's condition and a careful consideration of the risks and benefits are essential in determining the most appropriate treatment strategy.
