Hidden Threat: Endothelial Dysfunction in Type 2 Diabetes Even with Healthy Arteries
"New research reveals how diabetes damages blood vessels, increasing heart risks even when arteries appear normal."
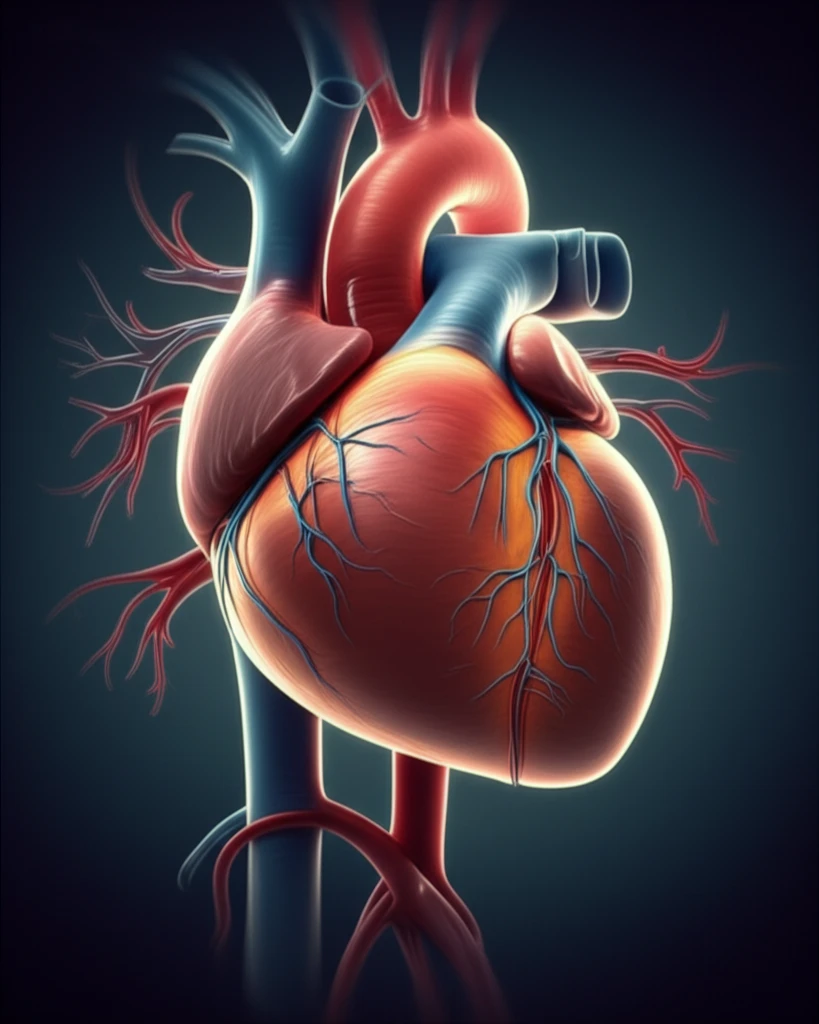
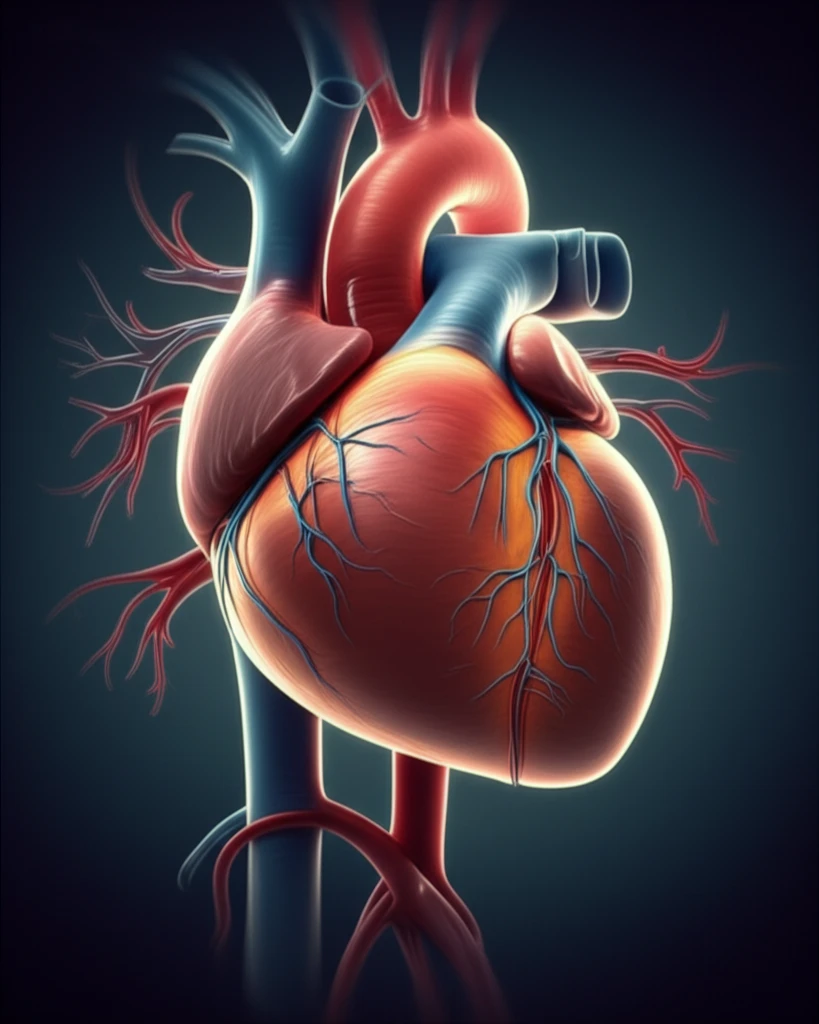
Endothelial dysfunction, a stealthy saboteur of cardiovascular health, acts as an early warning sign of atherosclerosis. It foreshadows potential coronary artery disease even before the telltale signs appear on angiograms. Prolonged exposure to cardiovascular risk factors messes with the endothelium, disrupting the production and metabolism of nitric oxide (NO) and ramping up the synthesis of reactive oxygen species (ROS). This leads to compromised endothelial integrity, setting the stage for atherosclerosis, thrombosis, and myocardial ischemia.
Initially identified in hypertensive individuals, endothelial dysfunction has since been found in type 1 and type 2 diabetes, coronary artery disease, and heart failure. Yet, its value as a therapeutic target, like other indicators of organ damage, remains somewhat undefined. Recent studies, however, underscore its role as a predictor of cardiovascular events, independent of coronary lesions. This has made assessing endothelial dysfunction a valuable tool for early risk stratification in patients susceptible to cardiovascular issues.
Consequently, novel non-invasive methods have been developed to assess endothelial function accurately, including flow-mediated dilation (FMD) of the brachial artery and, more recently, peripheral artery tonometry (PAT). These methods provide ways to detect early signs of vascular damage, allowing for more proactive interventions.
What is Peripheral Artery Tonometry (PAT) and Why Is It Important?
Peripheral artery tonometry (PAT) is a non-invasive technique used to evaluate endothelial function by measuring the pulsatile volume changes in the digital arteries. This method employs pneumatic probes attached to the fingertips to record these changes, offering a practical way to assess vascular health. PAT measures reactive hyperemia, the increase in blood flow after a period of ischemia, to determine how well the blood vessels are functioning. This is crucial because endothelial dysfunction can be an early indicator of cardiovascular disease.
- Non-Invasive Assessment: PAT provides a non-invasive way to assess endothelial function, making it a safer option than invasive methods.
- Predictive Capability: Studies have shown that PAT can predict future cardiovascular events, aiding in early risk stratification.
- Correlation with Other Methods: PAT results correlate well with other measures of endothelial function, validating its accuracy.
- Streamlined Approach: Compared to FMD, PAT is easier to perform and requires less expertise, making it more accessible.
What Does This Mean for Managing Diabetes?
In type 2 diabetes patients, endothelial function is significantly compromised compared to non-diabetic controls, even when other risk factors are similar. This helps explain the pathophysiologic impact of DM on coronary atherosclerosis development and its complications. This study shows that PAT is a valid tool for the early identification of endothelial dysfunction, with potential for use in large populations at cardiovascular risk. The findings support proactive monitoring and management of vascular health in diabetic patients to mitigate long-term cardiovascular risks.
