Heart Health Revolution: Innovative Treatments Reshape Cardiac Care
"Explore the latest advancements in cardiac treatments, from magnesium scaffolds to cutting-edge valve therapies, offering new hope for patients worldwide."
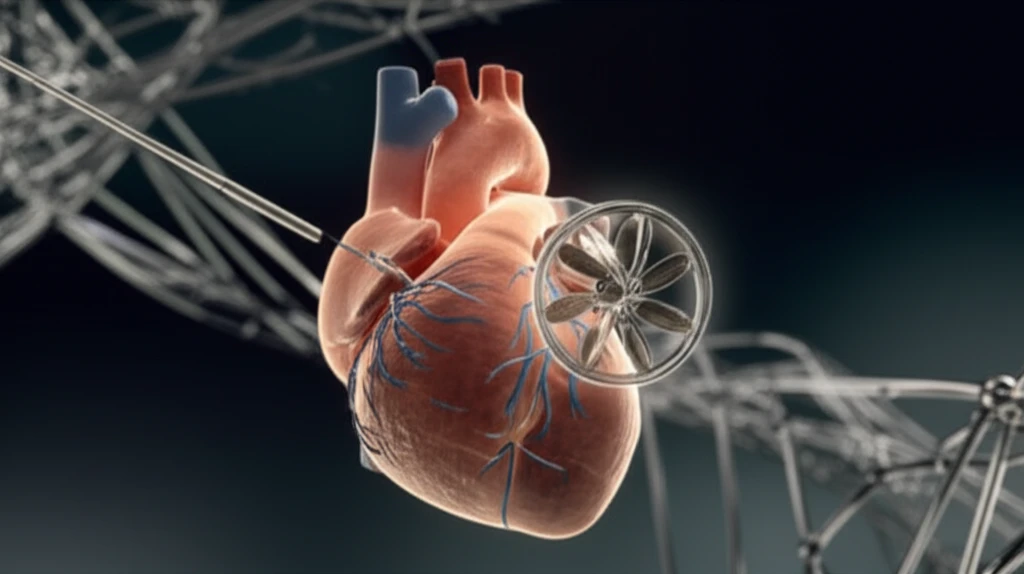
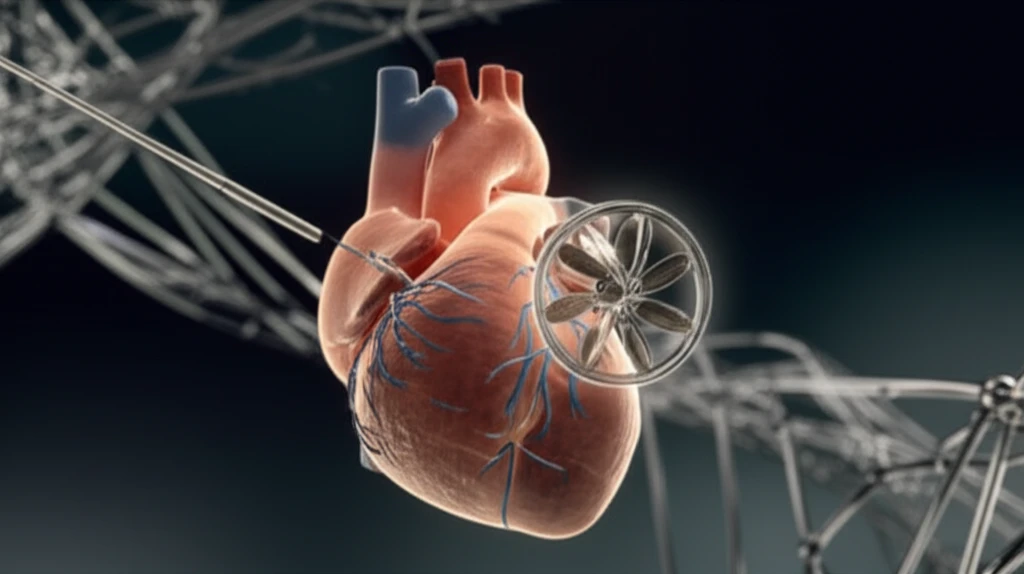
The landscape of cardiac care is undergoing a significant transformation, driven by groundbreaking innovations and technological advancements. These developments promise to enhance treatment efficacy, reduce patient risk, and improve overall outcomes for individuals facing a range of heart conditions. Let's delve into some of the most exciting breakthroughs that are reshaping the future of cardiology.
One promising area of advancement is the development of bioabsorbable magnesium scaffolds. Traditional drug-eluting stents (DES), while effective, have limitations in fully realizing the 'leave nothing behind' concept. However, innovative magnesium scaffolds are emerging as a potential solution, offering improved mechanical handling and a shorter resorption time. These scaffolds aim to minimize complications and promote better long-term healing.
Beyond scaffolds, transcatheter aortic valve implantation (TAVI) has revolutionized the treatment of severe aortic stenosis, particularly for high-risk patients who are not suitable candidates for open-heart surgery. TAVI procedures have seen exponential growth in recent years, driven by advancements in techniques, improved device designs, and better patient selection. This minimally invasive approach offers a less invasive alternative with comparable mortality rates to traditional valve replacement.
Magnesium Scaffolds: A New Dawn for Stent Technology?
Magnesium scaffolds represent a significant leap forward in stent technology. Unlike traditional metal stents that remain permanently implanted, magnesium scaffolds are designed to dissolve naturally over time. This bioabsorbable property offers several potential advantages, including reduced risk of long-term complications such as stent thrombosis and restenosis. Moreover, magnesium's biocompatibility promotes better vessel healing and reduces inflammation.
- Shorter Resorption Time: Dissolves within six to twelve months.
- Improved Handling: Easier to deploy compared to polylactid scaffolds.
- Promising Clinical Data: BIOSOLVE-II study shows favorable outcomes with reduced lumen loss.
- Minimal Hyperplasia: Intravascular ultrasound shows minimal neointimal hyperplasia.
Transforming Aortic Stenosis Treatment: The Rise of TAVI
TAVI has emerged as a game-changing alternative to traditional surgical aortic valve replacement, especially for patients deemed high-risk or inoperable. This minimally invasive procedure involves inserting a new valve through a catheter, typically inserted through the femoral artery. The TAVI procedure has several benefits, including shorter hospital stays, quicker recovery times, and reduced risk of complications compared to open-heart surgery. As TAVI technology continues to advance and patient selection criteria expand, it is poised to become the standard of care for a broader range of patients with aortic stenosis.
