Heart Health Breakthrough: Can Off-Pump Bypass Surgery Help Those With Weak Hearts?
"Discover how a modified heart surgery technique is giving new hope to patients with severe heart failure."
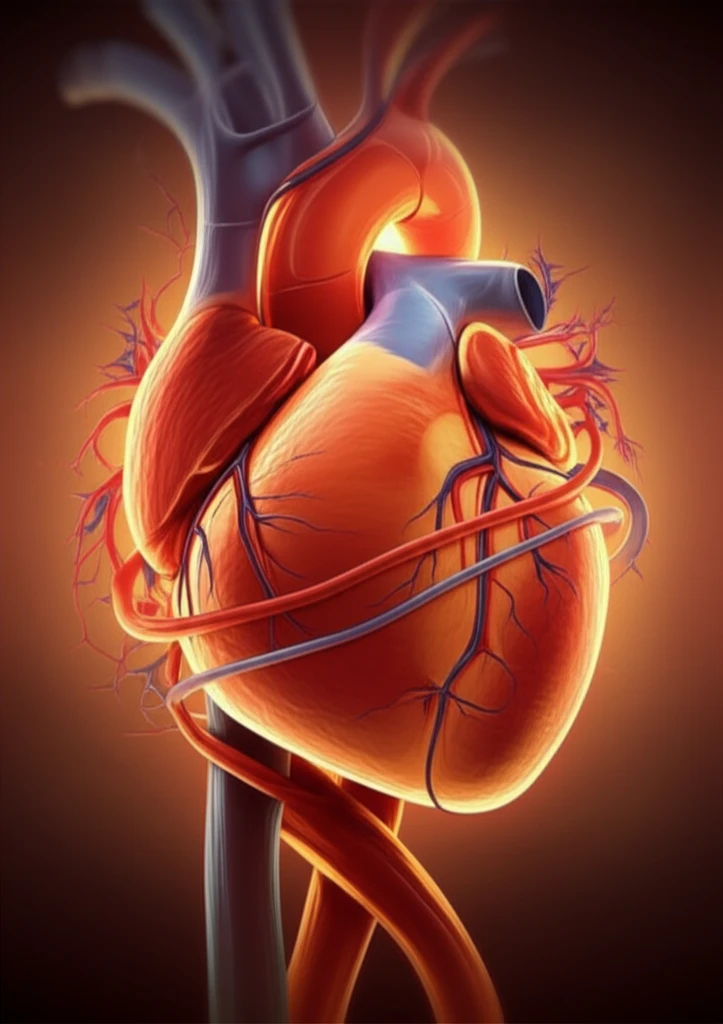
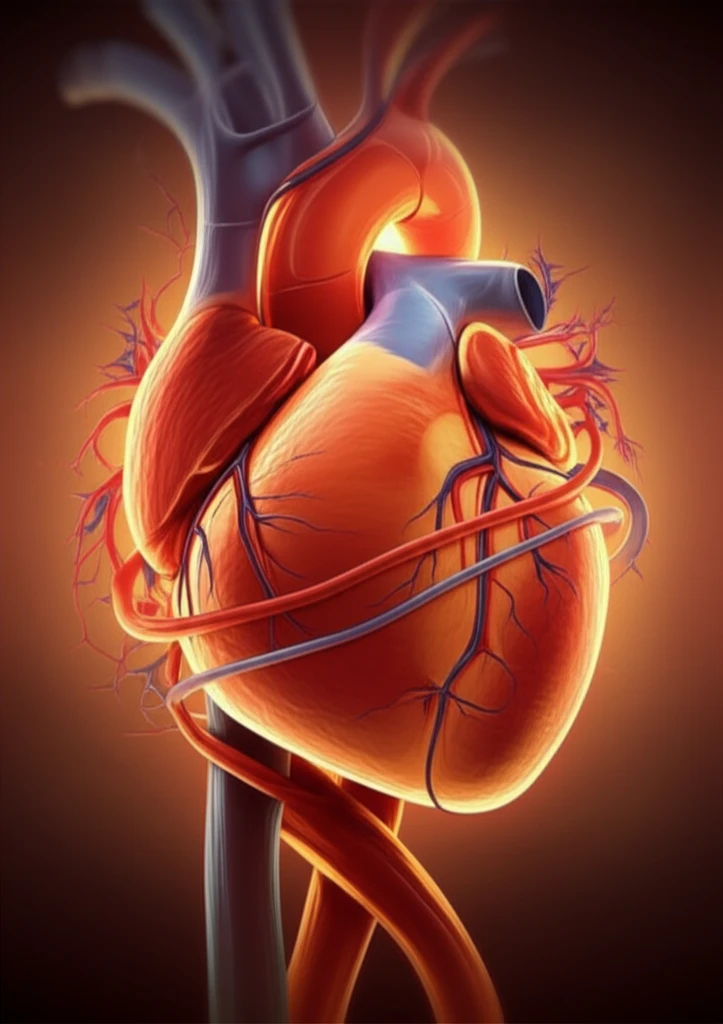
For individuals grappling with severe left ventricular (LV) dysfunction, a condition where the heart struggles to pump blood effectively, coronary artery bypass surgery presents a significant challenge. But, the evolution of surgical methods, particularly the rise of off-pump coronary artery bypass (OPCAB) surgery, offers a beacon of hope.
OPCAB has emerged as a compelling alternative to traditional bypass surgery, which relies on cardiopulmonary bypass machines. OPCAB allows surgeons to operate on a beating heart, reducing the risks associated with stopping and restarting the heart. Furthermore, studies suggest that using bilateral internal thoracic arterial grafts, which utilize arteries from the chest wall, provides superior long-term outcomes compared to single grafts.
Although OPCAB with bilateral internal thoracic arterial grafting shows promise for patients, understanding the specific outcomes remains crucial. This article will explore how patients with severe left ventricular dysfunction fare with this innovative surgical approach, comparing their results to those with better heart function.
OPCAB: A Promising Option for LV Dysfunction?
A study published in the Journal of Korean Medical Science, explored the outcomes of OPCAB with composite bilateral internal thoracic artery grafting in patients with varying degrees of left ventricular function. The researchers aimed to determine if this approach could effectively improve outcomes for those with severely compromised hearts.
- Patient Population: The study included a diverse group of patients undergoing OPCAB, allowing for a comparison of outcomes based on the severity of LV dysfunction.
- Surgical Technique: All patients received composite bilateral internal thoracic artery grafts, a technique known for its potential long-term benefits.
- Outcome Measures: The study analyzed early and late mortality, cardiac events, and changes in left ventricular function to assess the effectiveness of OPCAB in different patient subgroups.
The Future of Heart Surgery
While the study highlights the potential benefits of OPCAB in patients with severe LV dysfunction, it also underscores the increased risk associated with this condition. Further research is needed to refine surgical techniques and identify strategies to mitigate these risks, ultimately improving long-term outcomes for individuals with weakened hearts. The findings suggest that OPCAB with bilateral internal thoracic artery grafting can be a valuable option, but careful patient selection and management are crucial.
