Gut Feeling Gone Wrong: How Lymphatic Traffic Jams Can Harm Your Brain
"New research reveals the surprising link between blocked lymph flow in your gut and increased brain inflammation after a stroke-like event."
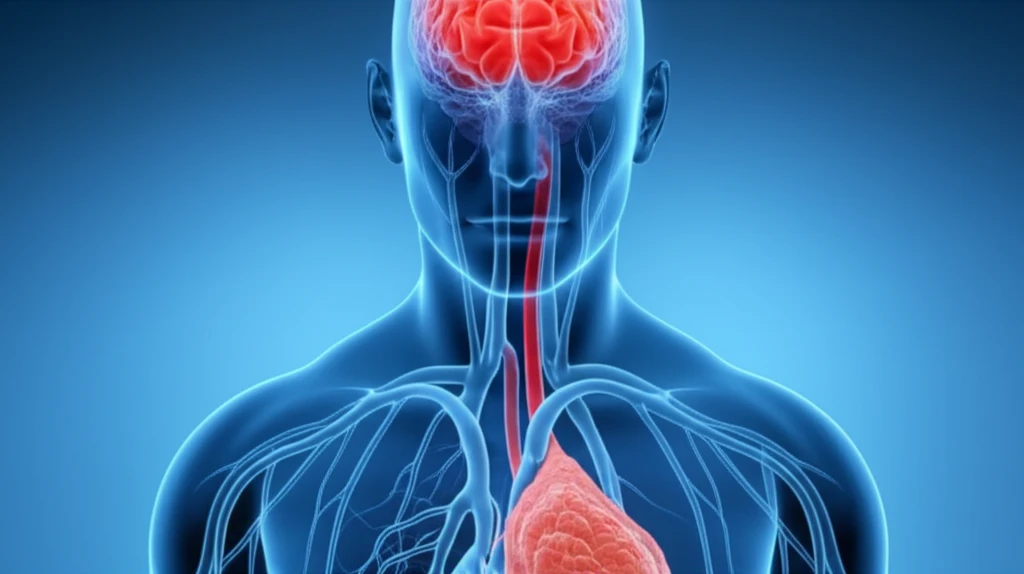
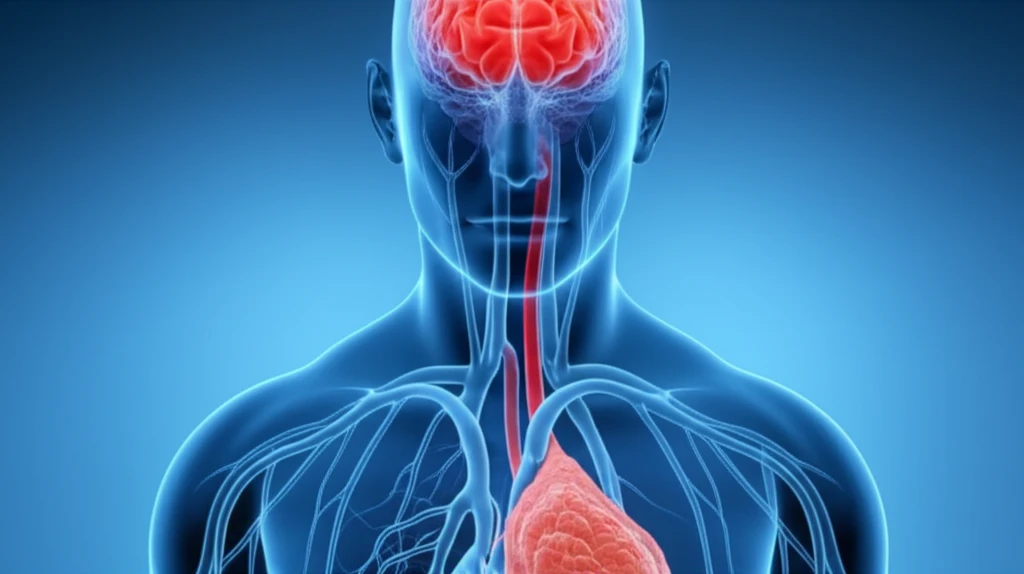
When a stroke occurs due to a blocked artery in the brain, it sets off a chain reaction. The initial blockage deprives the brain of oxygen and nutrients, leading to immediate damage. However, the problems don't stop there. What follows, known as ischemia-reperfusion injury, can sometimes cause even more harm than the initial event.
Scientists are increasingly focused on the gut's role in overall health, and it turns out that problems in the gut can make brain injuries worse. A key player in this connection is the mesenteric lymphatic system, a network of vessels that drains fluid and waste from the intestines. If this drainage system gets blocked, it can lead to serious consequences for the brain after a stroke-like event.
This article explores groundbreaking research that uncovers how a backup of lymphatic fluid in the gut can intensify brain inflammation and damage following a stroke. We'll break down the science in a way that's easy to understand, revealing the hidden dangers of a poorly functioning gut lymphatic system and what it could mean for future treatments.
The Gut-Brain Link: Why a Blocked Lymph System Spells Trouble
The study, conducted on rats, investigated what happens when the mesenteric lymph duct (MLD) is blocked during a stroke-like event called superior mesenteric artery occlusion (SMAO). Researchers created four groups: one with a blocked MLD, one with SMAO, one with both, and a control group. They then measured levels of endotoxins (harmful substances released by bacteria) and inflammatory markers in the brain.
- Endotoxin Levels: Significantly increased in the brains of rats with both SMAO and blocked MLD.
- Inflammatory Markers (CD14, LBP, ICAM-1, TNF-α): These markers, which indicate inflammation, were also much higher in the combined SMAO and blocked MLD group.
- The Culprit: Blocking the MLD appears to exacerbate the translocation of endotoxins from the gut to the brain, triggering a stronger inflammatory response.
What Does This Mean for You? The Future of Stroke Recovery
This research highlights the critical connection between gut health and brain health, particularly in the context of stroke recovery. While more research is needed, these findings suggest that maintaining a healthy gut lymphatic system could be a crucial factor in minimizing brain damage after a stroke.
What can you do? Focus on lifestyle choices that promote a healthy gut, such as eating a balanced diet rich in fiber, staying hydrated, and managing stress. If you're at risk for stroke or have a history of stroke, talk to your doctor about strategies to support your gut health.
In the future, treatments that target the gut lymphatic system could become a promising avenue for improving stroke outcomes. By addressing the root cause of inflammation and preventing the translocation of harmful substances to the brain, we may be able to unlock new possibilities for recovery and rehabilitation.
