Gastric Foregut Cysts: Unraveling a Diagnostic Puzzle
"Learn about the latest insights into gastric foregut cystic malformations, a rare condition often mistaken for other tumors, and how accurate diagnosis can improve surgical outcomes."
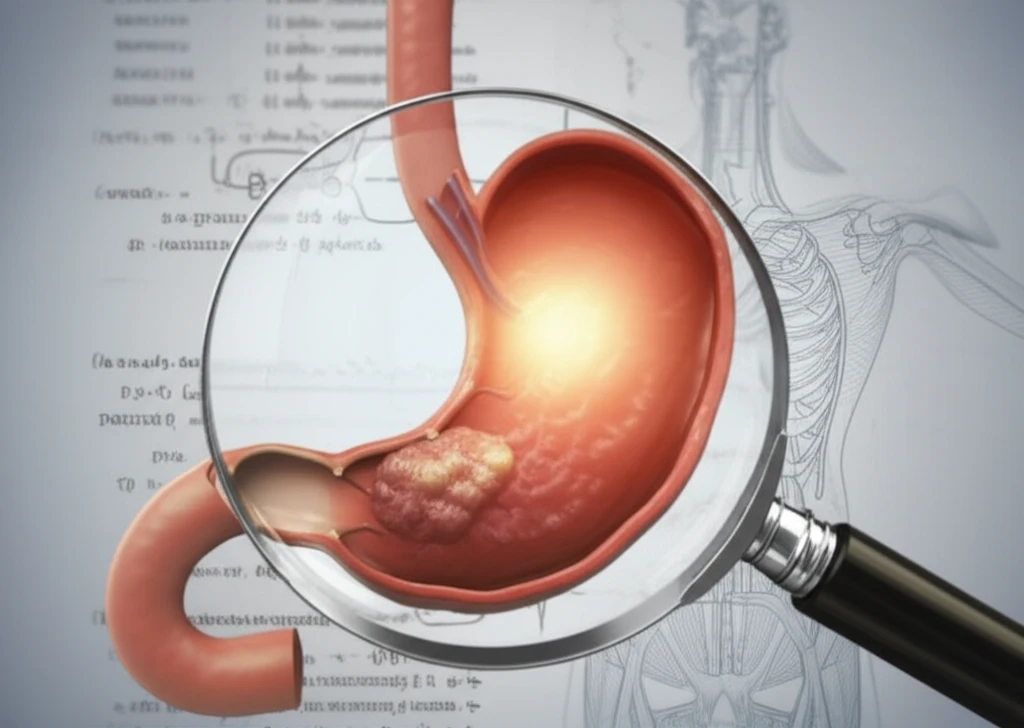
Gastric foregut cystic developmental malformations (G-FCDMs) are rare lesions in the alimentary tract, particularly the stomach. These cysts pose diagnostic challenges due to their similarity to other conditions, such as gastric duplication cysts and bronchogenic cysts. Accurate identification is crucial for appropriate surgical management.
Historically, the nomenclature for these cysts has been inconsistent, leading to confusion. While gastric duplication cysts involve gastric mucosa and submucosal glands, bronchogenic cysts feature respiratory mucosa with cartilage and glands. G-FCDMs, however, lack these specific tissues, presenting pseudostratified ciliated columnar epithelium (PCCE).
Recent research, including a detailed case series and literature review, sheds light on the clinical and embryological characteristics of G-FCDMs. This article delves into these findings, providing insights to differentiate G-FCDMs from other gastric lesions, optimize diagnostic accuracy, and improve surgical outcomes.
Decoding Gastric Foregut Cystic Malformations: What Sets Them Apart?
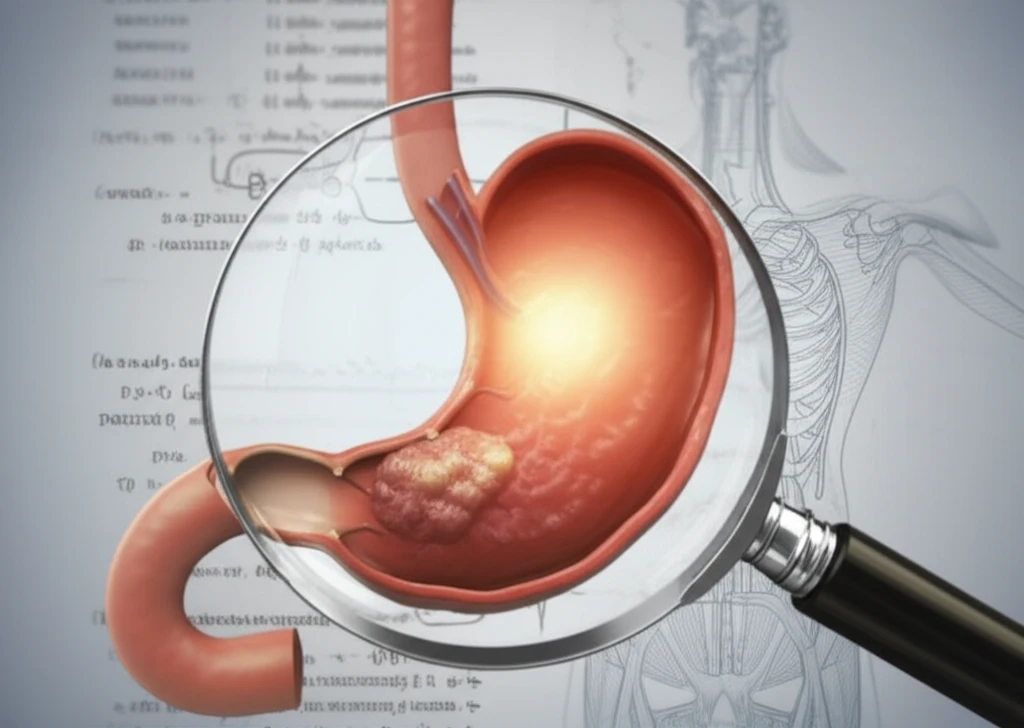
Distinguishing G-FCDMs from other gastric lesions requires careful consideration of their unique features. Key differences lie in their histological composition and embryological origins.
- Gastric Duplication Cysts: Contain gastric mucosa and submucosal glands.
- Bronchogenic Cysts: Feature respiratory mucosa with underlying cartilage and glands.
- G-FCDMs: Lack gastric mucosa, glands, or cartilage, presenting pseudostratified ciliated columnar epithelium (PCCE).
Improving Outcomes: The Importance of Accurate Diagnosis
Preoperative recognition of G-FCDMs remains infrequent, leading to potential misdiagnosis and inappropriate surgical approaches. A lack of understanding regarding their embryologic origins further contributes to this challenge.
However, accurate presurgical identification of G-FCDMs is crucial for optimizing patient outcomes and minimizing complications. Advanced diagnostic techniques, such as endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA), can aid in confirming the diagnosis.
By enhancing awareness and understanding of G-FCDMs, clinicians can improve diagnostic accuracy, guide appropriate surgical management, and ultimately enhance the well-being of patients with these rare lesions.
