Fetal Membranes: Nature's Regenerative Toolkit for Modern Medicine
"Unlocking the Healing Powers of Birth Tissues: From Ancient Remedies to Cutting-Edge Therapies"
For nearly a century, fetal membranes, the tissues that surround and protect a developing baby, have been quietly utilized in medicine. What started as a simple technique for skin dressings has evolved into a promising field of regenerative medicine, thanks to the discovery of unique stem cell populations within these tissues.
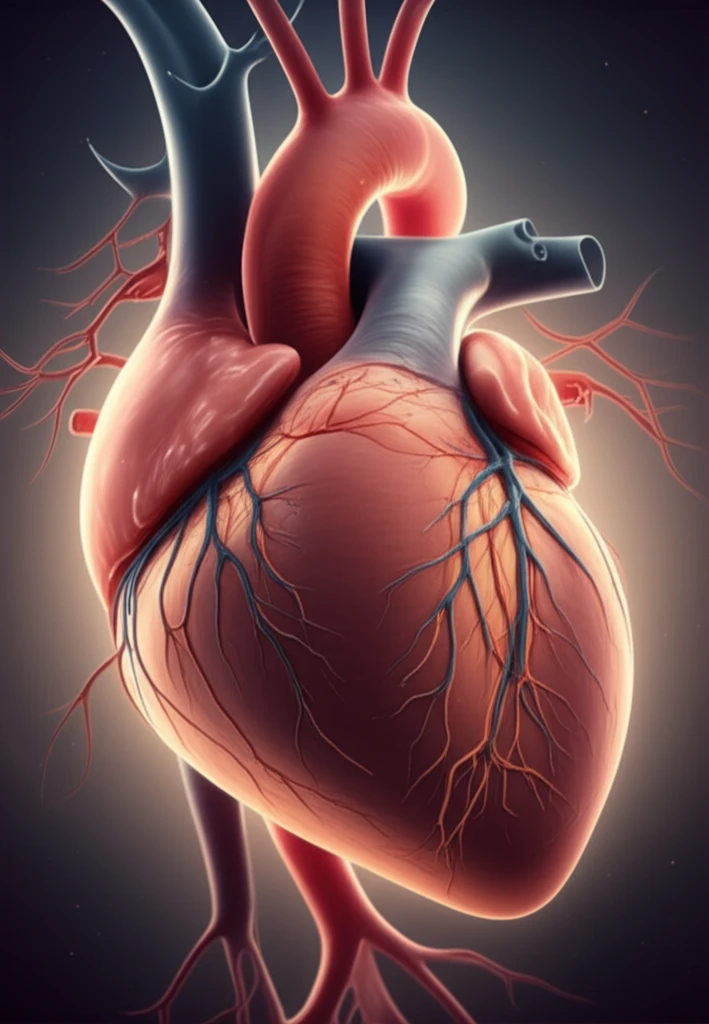
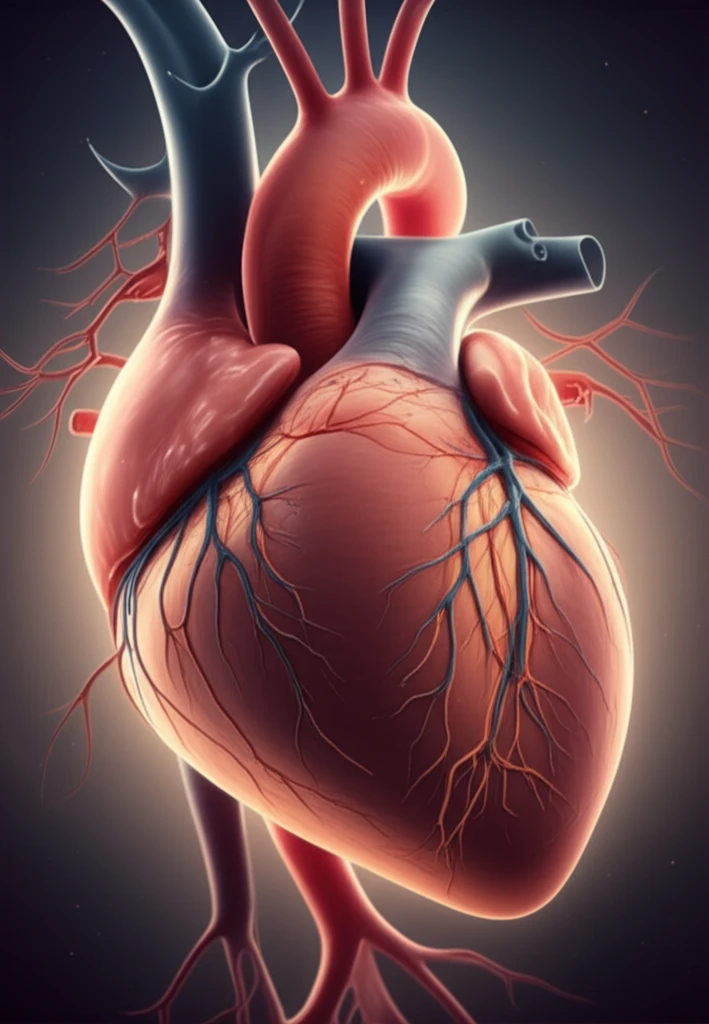
These stem cells, along with the inherent biological properties of the fetal membranes themselves, offer a unique combination of pro-angiogenic (promoting blood vessel growth) and immunomodulatory (regulating the immune system) effects. Researchers are now exploring how these properties can be harnessed to treat a wide range of conditions.
This article delves into the fascinating history of fetal membrane use, explores their biological origins and function, and highlights recent advancements in utilizing fetal membranes and their derived stem cells for regenerative therapies.
The Science Behind the Sac: How Fetal Membranes Promote Healing
During pregnancy, the placenta plays a vital role in modulating the mother's immune system to protect the developing fetus. The fetal membranes, which comprise the amniotic and chorionic membranes, are key players in this process. They create an immunological barrier between mother and child.
- Immunomodulation: Fetal membranes help switch the maternal immune system from surveillance to tolerance, creating a safe environment for the fetus to grow.
- HLA-G Expression: High levels of HLA-G on fetal membranes play a critical role in maternal-fetal tolerance.
- Barrier Function: Trophoblasts act as an immunological barrier, preventing the mother's immune cells from directly attacking the fetus.
The Future is Fetal: Charting the Course for Clinical Translation
Fetal membranes have transitioned from simple wound coverings to a source of stem cells and advanced therapies. Their unique immunological properties and regenerative potential make them valuable assets in treating a wide range of conditions, from burns and corneal damage to cardiovascular and neurological disorders.
Several early-phase clinical trials are already underway, investigating the safety and efficacy of fetal membrane-derived stem cells. The results of these trials will be crucial in shaping the future of this field and guiding the development of new regenerative medicine strategies.
To fully realize the potential of fetal membranes, it is essential to continue researching their biological roles during pregnancy and fetal wound healing. By understanding their microenvironment and mechanisms of action, we can optimize cell priming protocols, design effective bioreactors for large-scale cell production, and ultimately translate these discoveries into widespread clinical applications.
