Facial Canal Dehiscence: Are You at Risk? What You Need to Know
"Understanding the causes, risks, and prevention of facial nerve damage during chronic otitis media surgery."
Imagine undergoing ear surgery only to face an unexpected complication: facial paralysis. This is a real concern for otolaryngologists (ENT surgeons) and patients dealing with chronic otitis media (COM), an ongoing ear infection. Facial nerve paralysis doesn't just affect physical appearance; it can lead to social isolation and a hit to one's self-esteem.
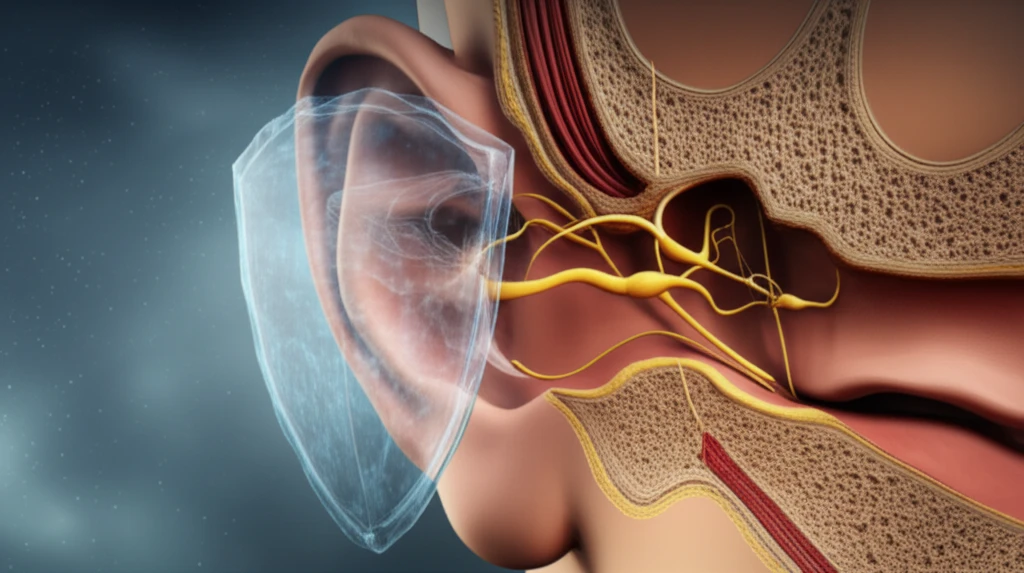
The culprit behind this complication can be a condition called Facial Canal Dehiscence (FCD). FCD refers to an absence of bone covering the facial nerve canal, leaving the nerve vulnerable during surgery. While a solid understanding of anatomy is crucial, surgeons also need to be aware of the possibility of FCD during ear operations to prevent nerve damage.
A recent study investigated the rate and location of FCD in patients undergoing surgery for chronic otitis media, both with and without cholesteatoma (a skin cyst in the middle ear). By understanding the prevalence and common locations of FCD, surgeons can take extra precautions to protect the facial nerve.
What is Facial Canal Dehiscence (FCD) and Why Does It Matter?
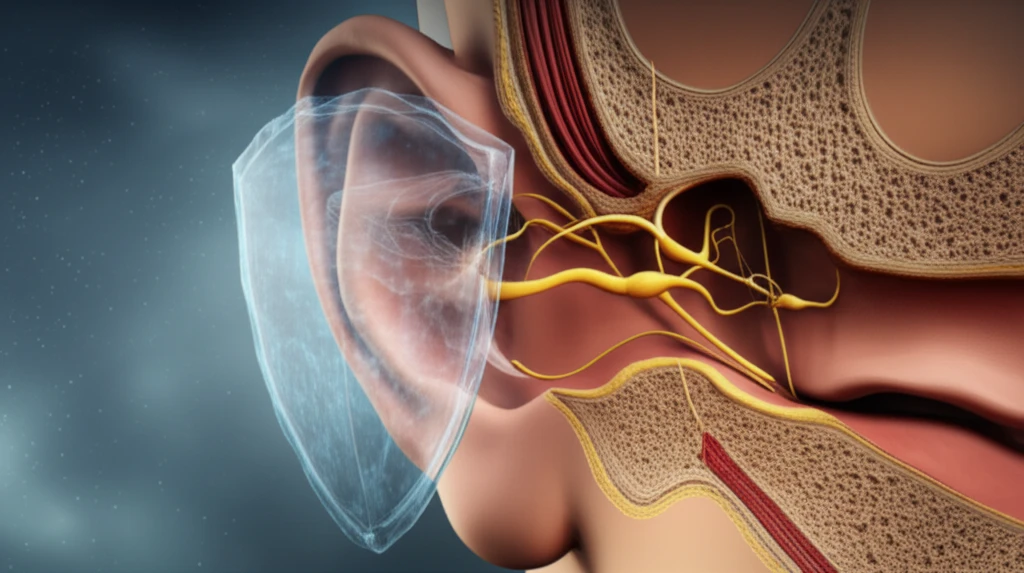
Facial Canal Dehiscence (FCD) is a condition where the bony covering of the facial nerve canal is missing. This leaves the facial nerve exposed and vulnerable to injury during ear surgeries. FCD can be present from birth or develop over time due to bone erosion caused by chronic ear infections, particularly those involving cholesteatoma.
- Prevalence: FCD was found in 11.29% of the patients.
- Association with Cholesteatoma: FCD was more common in patients with cholesteatoma (88.1%) compared to those without (11.9%).
- Location: The most frequent location of FCD was in the tympanic segment (76.19%) of the facial canal, which is near the oval window.
- Ossicular Erosion: In cases where FCD was present, erosion of all three ossicles (small bones in the middle ear) was statistically more frequent.
Protecting the Facial Nerve: What Surgeons Can Do
The study emphasizes the need for surgeons to be extra vigilant when operating on patients with chronic otitis media, especially those with cholesteatoma. Given that FCD is most commonly found near the oval window, careful examination of this area is crucial.
The study suggests that if the stapes (one of the ossicles) or all three ossicles are eroded, the risk of FCD is higher. Surgeons should exercise extreme caution in these situations to minimize the risk of facial nerve injury.
While preoperative imaging, such as micro-CT scans, can help identify FCD, the ultimate determination often relies on careful intraoperative examination. By staying informed about the prevalence, location, and associated factors of FCD, surgeons can enhance their ability to protect the facial nerve and improve patient outcomes.
