EUS vs. ERCP: Choosing the Right Drainage Method for Biliary Obstruction
"A closer look at the efficacy and safety of EUS-guided and ERCP-guided biliary drainage for treating malignant obstructions."
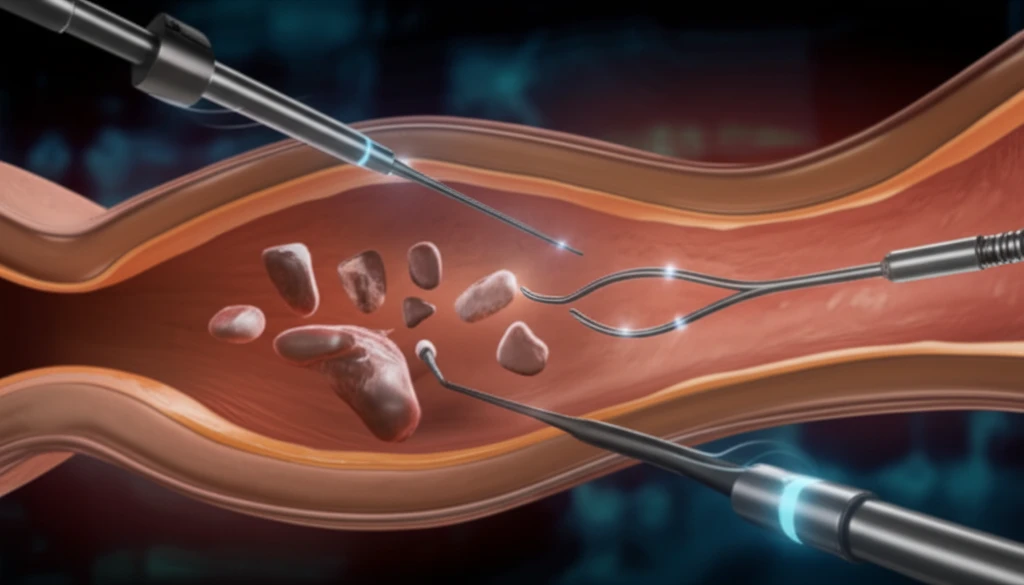
Biliary obstruction, a condition where the bile ducts become blocked, can lead to serious health issues if left untreated. Malignant biliary obstruction, often caused by tumors, requires effective drainage to relieve symptoms and improve patient outcomes.
Traditionally, endoscopic retrograde cholangiopancreatography (ERCP) has been the standard approach for biliary drainage. However, endoscopic ultrasound-guided biliary drainage (EUS-BD) has emerged as a promising alternative. The choice between EUS and ERCP depends on various factors, including the location and nature of the obstruction, as well as the patient's overall health.
Recent studies, including a prospective randomized trial by Park et al., have compared the efficacy and safety of EUS-BD and ERCP-BD. While the initial findings suggested similar safety profiles, ongoing discussions and further research are crucial to fully understand the advantages and limitations of each method. This article delves into the nuances of these drainage techniques, offering insights to help patients and healthcare providers make informed decisions.
EUS-BD vs. ERCP-BD: Understanding the Key Differences
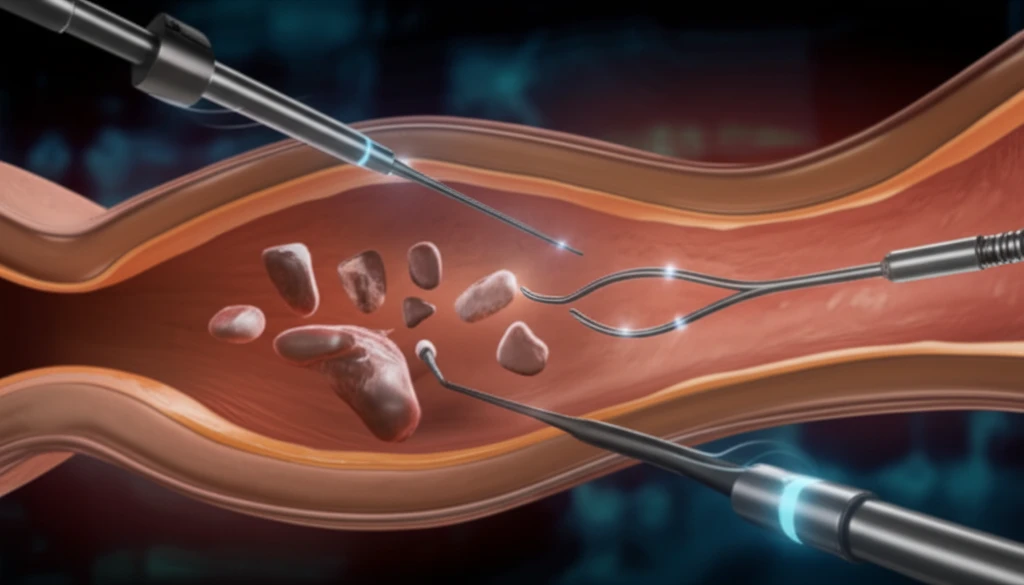
ERCP involves inserting an endoscope through the mouth, esophagus, and stomach to reach the bile ducts. A catheter is then guided into the bile duct, and contrast dye is injected to visualize the obstruction. If necessary, a stent can be placed to keep the duct open.
- Accessibility: EUS-BD may be preferred when ERCP is not feasible due to anatomical variations or prior surgery.
- Success Rates: Both methods have high success rates, but EUS-BD may be more successful in certain situations.
- Adverse Events: While both procedures carry risks, the types and frequencies of adverse events can differ.
- Stent Patency: The longevity of the stent's functionality can influence the choice between EUS and ERCP.
Making Informed Decisions About Biliary Drainage
Choosing between EUS-BD and ERCP-BD requires careful consideration of individual patient factors, the expertise of the medical team, and the available resources. As research continues to evolve, staying informed and discussing all options with your healthcare provider is essential for achieving the best possible outcome in managing biliary obstruction.
