Endotension: The Silent Threat in Aortic Aneurysm Repair
"Unveiling the complexities of endotension after endovascular aneurysm repair (EVAR) and how it leads to rupture."
For patients with aortic aneurysms who are not candidates for conventional surgery or standard endovascular procedures, a new technique called 'chimney' is considered. This approach involves placing stents through the visceral and renal branches of the aorta during endovascular aneurysm repair (EVAR).
The 'chimney' technique is used when open surgery carries significant risks because the aneurysm affects the renal and visceral vessels. It involves deploying covered stents parallel to the main aortic stent-graft to maintain blood flow to vital side branches.
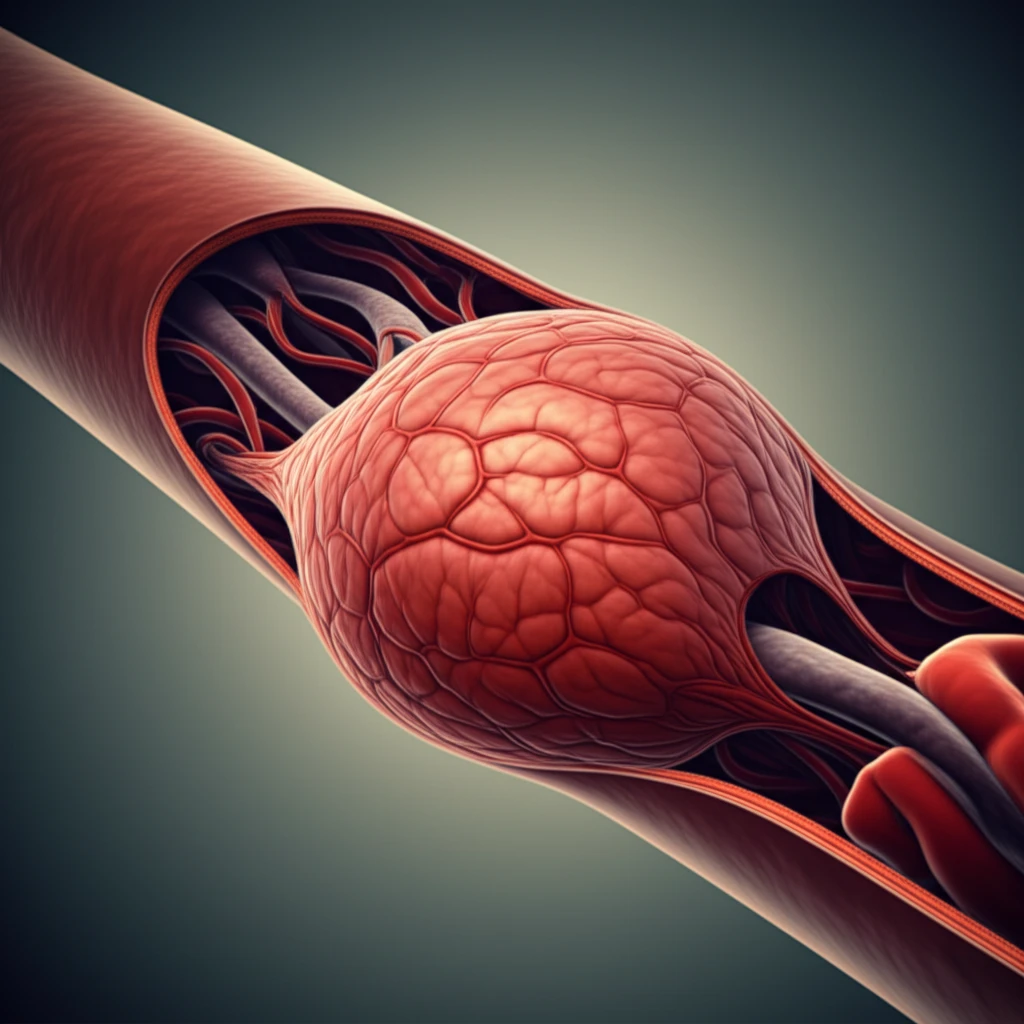
While EVAR has become a routine procedure, it isn't without potential complications. One of the most common of these is an endoleak, where blood flow persists within the excluded aneurysm sac, pressurizing it and increasing the risk of rupture. This article will guide you through understanding of endoleaks and endotension, and the best ways to protect yourself.
What is Endotension?
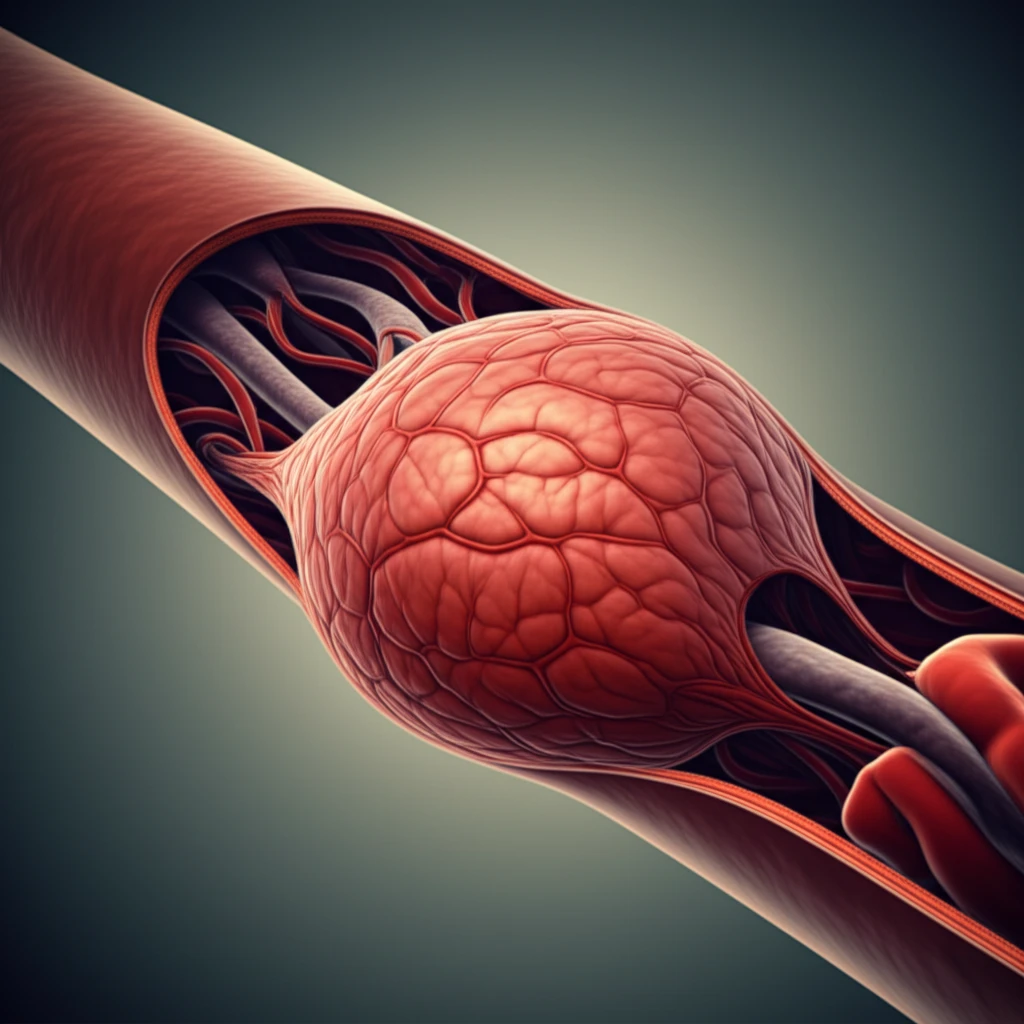
An endoleak is a complication of EVAR, maintaining flow and pressure within the excluded aneurysm sac. Endoleaks are classified into five types based on their mechanisms and locations.
- Type I: Occurs at the proximal or distal attachment sites of the endograft, indicating an incomplete seal.
- Type II: Results from retrograde flow into the aneurysm sac via branch vessels like the lumbar or inferior mesenteric arteries.
- Type III: Involves leaks due to graft defects, disconnection of graft components, or tears in the graft material.
- Type IV: Characterized by graft porosity, where blood permeates through the graft fabric itself.
- Type V (Endotension): Aneurysm sac expansion without a detectable leak, often due to increased pressure transmitted through the thrombus lining the sac.
Navigating the Shadows of Endotension
The development of aneurysm sac expansion due to endotension remains a diagnostic challenge, even with advanced imaging techniques. Because endotension lacks visible leaks, it requires a high degree of clinical suspicion and often is diagnosed by exclusion. Continued research into new diagnostic methods, such as implantable pressure sensors, is essential to improving outcomes and reducing the risk of rupture in patients undergoing EVAR.
