Diaphragmatic Hernia After Liver Cancer Treatment: What You Need to Know
"A rare complication of radiofrequency ablation, diaphragmatic hernias can develop months after treatment for hepatocellular carcinoma. Understanding the risks and management is key."
Radiofrequency ablation (RFA) has become a popular treatment for hepatocellular carcinoma (HCC) due to its safety and effectiveness in eradicating tumor cells. RFA involves using heat to destroy cancerous tissue. While generally considered safe and minimally invasive, RFA can sometimes lead to serious complications.
One such rare complication is diaphragmatic hernia, where abdominal organs protrude through an opening in the diaphragm. This condition can occur months after the RFA procedure, making it crucial for patients and healthcare providers to be aware of the potential risks and symptoms.
This article explores a case of diaphragmatic hernia that developed after RFA treatment for HCC. It provides insights into the possible causes, symptoms, diagnosis, and management of this unusual complication.
Understanding Diaphragmatic Hernia After RFA
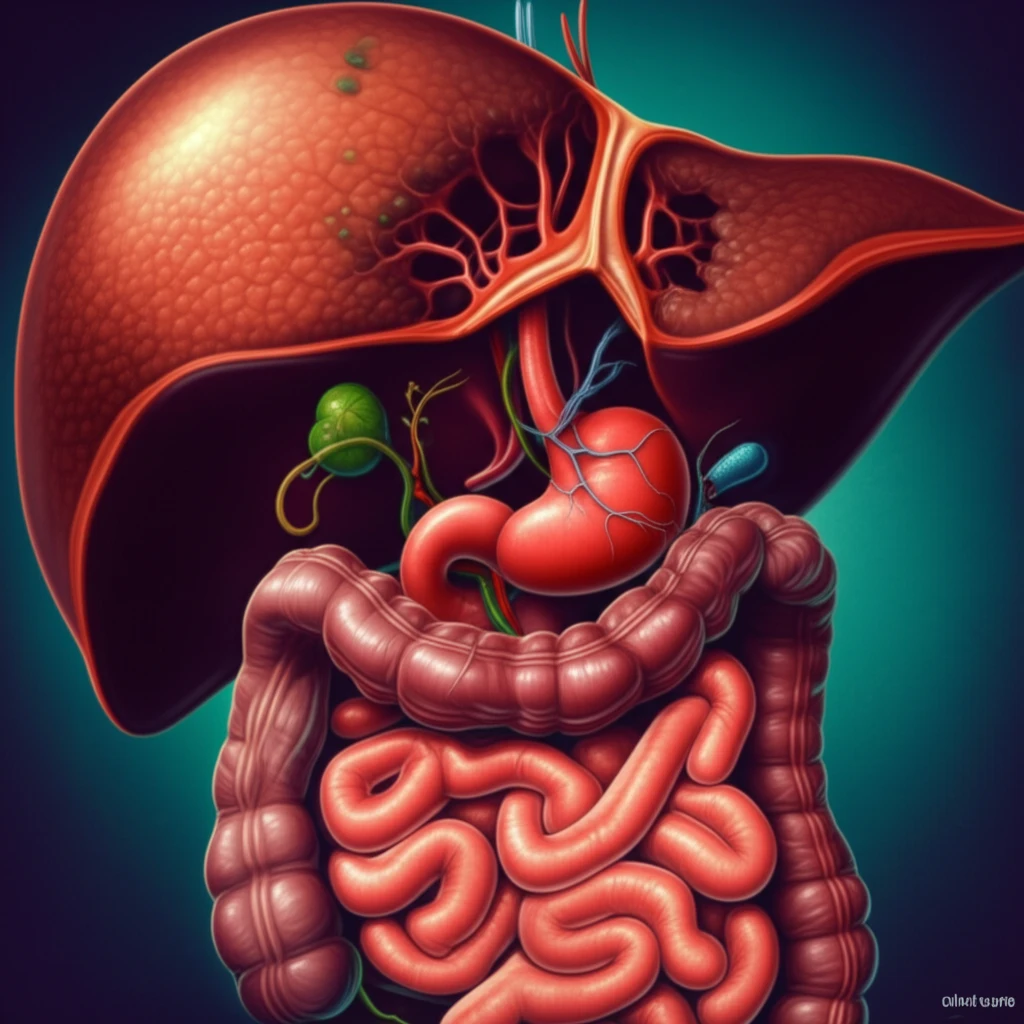
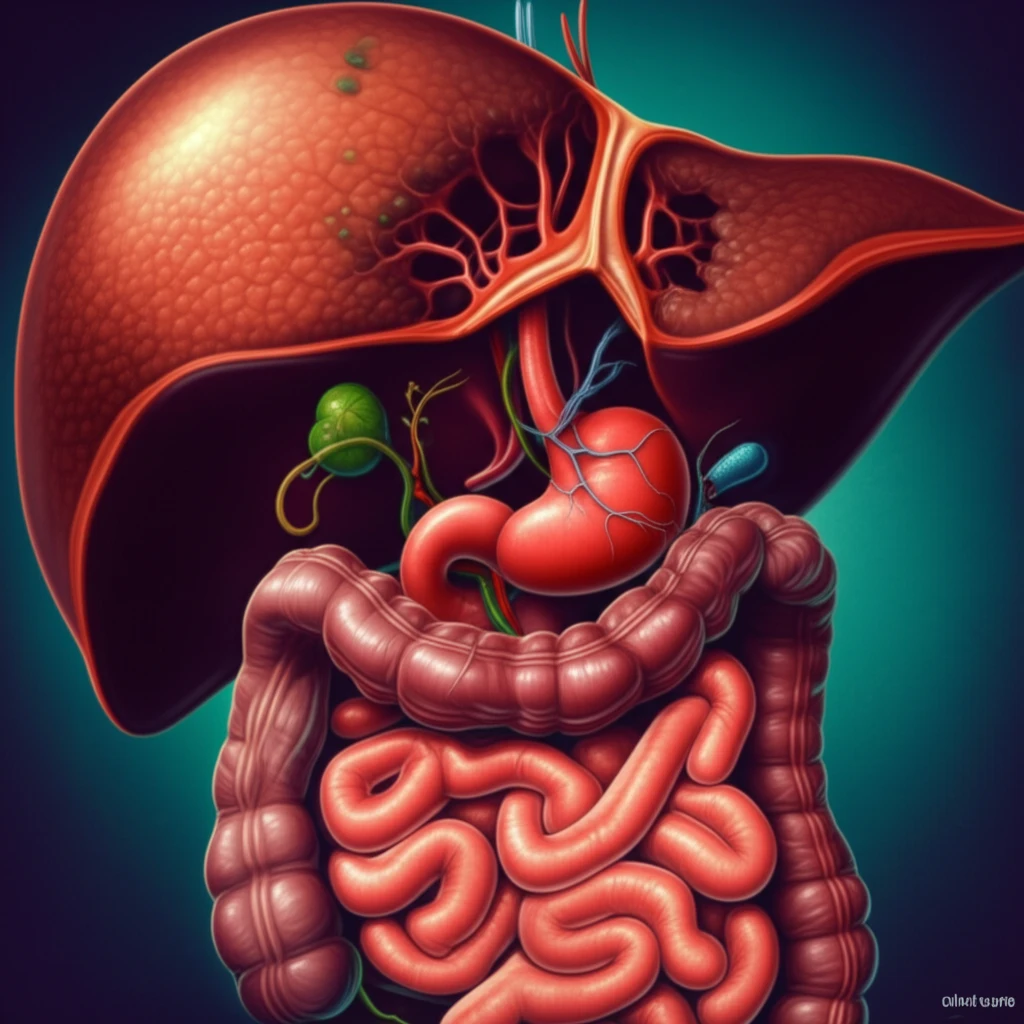
A diaphragmatic hernia occurs when there's a defect in the diaphragm, the muscle separating the chest and abdominal cavities. This allows abdominal organs, such as the intestines or stomach, to push through into the chest cavity. While some diaphragmatic hernias are congenital (present at birth), others can be acquired due to trauma or medical procedures.
- Thermal Damage: The heat from RFA can directly injure the diaphragm, weakening its structure.
- Inflammatory Response: The body's inflammatory response to the thermal injury may further contribute to tissue damage and weakening.
- Compromised Healing: Conditions like diabetes mellitus or poor liver function might impair the healing process in the injured diaphragm, increasing the risk of hernia formation.
Key Takeaways & Considerations
While diaphragmatic hernia after RFA for HCC is rare, it's essential for patients and healthcare providers to be aware of this potential complication. Early detection and appropriate management can help prevent serious consequences.
If you've undergone RFA for HCC, be vigilant for any new or worsening symptoms such as chest pain, shortness of breath, or abdominal discomfort. Regular follow-up imaging can also help detect diaphragmatic defects early on.
If you're a candidate for RFA for HCC, discuss the potential risks and benefits with your healthcare provider. Techniques like artificial pleural effusion or ascites, and carbon dioxide insufflation may help to minimize thermal injury to the diaphragm during the procedure. In summary, while RFA is a valuable tool in treating liver cancer, being informed about potential complications empowers patients and providers to make the best decisions for their care.
