Depression's Silent Battle: How Stress Fuels Prostate Cancer's Growth
"New research reveals the hidden link between mental health, inflammation, and the progression of prostate cancer."
October 26, 2023 - Prostate cancer, a disease affecting millions of men worldwide, presents a complex challenge. But what if something beyond the typical risk factors—age, genetics, and lifestyle—was also playing a crucial role? Recent research sheds light on a startling connection: the link between depression, the body's immune response, and the accelerated growth of prostate cancer. This groundbreaking discovery opens new avenues for understanding the disease and highlights the importance of addressing mental health in cancer treatment.
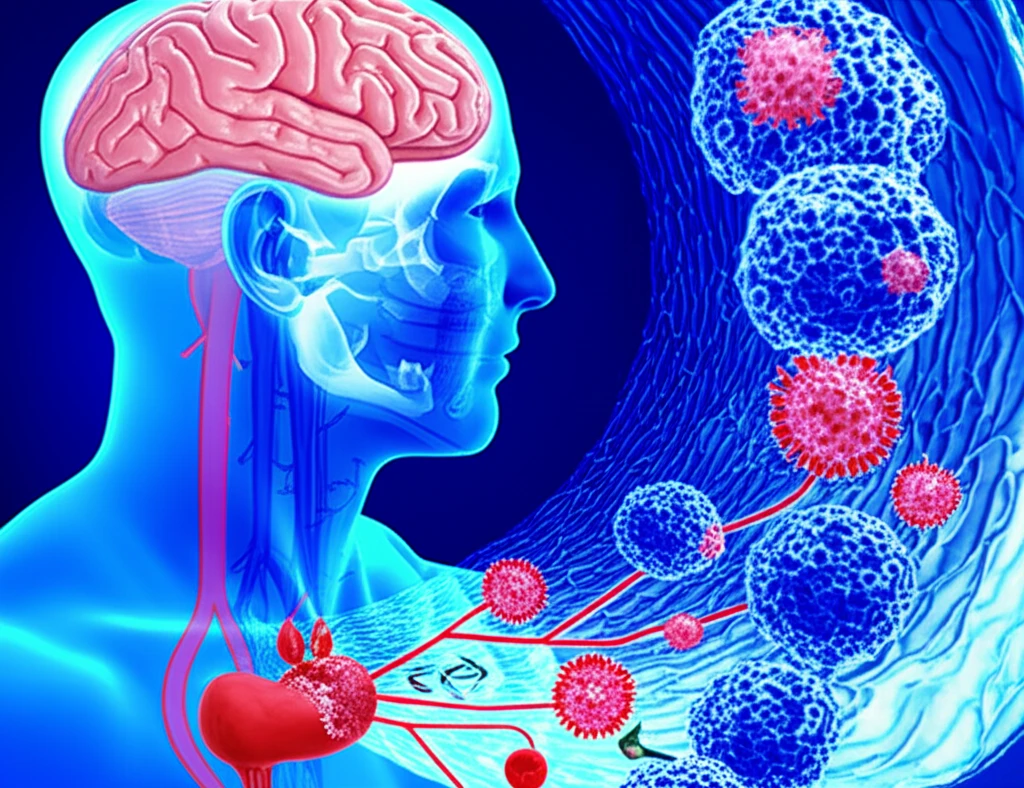
The human body is a complex ecosystem, and mental health profoundly influences physical health. Chronic stress and depression are known to trigger systemic inflammation, a known driver of cancer progression. The latest studies delve into the specific mechanisms by which depression impacts the microenvironment of prostate tumors, revealing how it recruits certain types of immune cells to promote cancer's expansion. These findings offer a deeper understanding of the disease and the potential for innovative treatment strategies.
This article explores the intricate relationship between depression and prostate cancer, offering a comprehensive overview of the latest research. We'll examine how the brain and the immune system interact in the context of cancer and discuss potential therapeutic interventions that target both the disease and the mental health challenges associated with it. This research provides vital insights for individuals, healthcare providers, and researchers working to improve outcomes for those affected by prostate cancer.
Unveiling the Connection: How Depression Alters the Immune Landscape
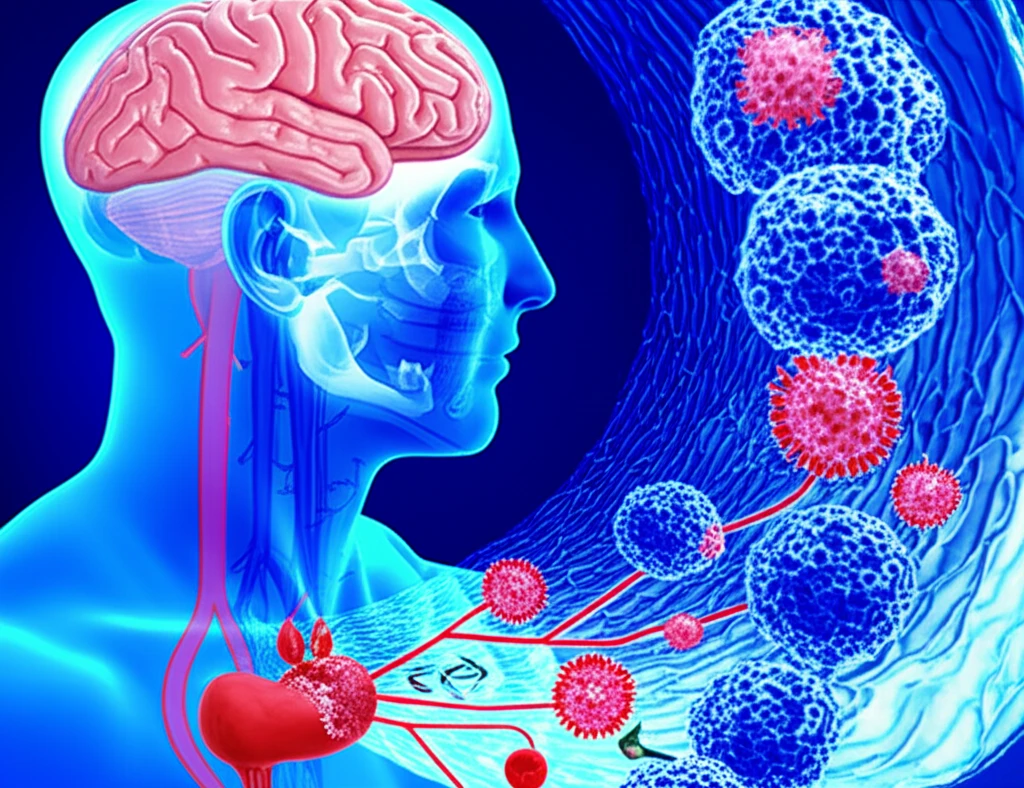
The study focused on how chronic stress, a key element of depression, influences the microenvironment of prostate tumors. The researchers discovered that depression activates the sympathetic nervous system, triggering an inflammatory response and encouraging tumor growth. They found that psychological stress leads to an increase in the levels of certain immune cells, particularly myeloid cells. These cells play a role in the body's defense mechanisms, and when they become dysregulated, they can inadvertently promote cancer.
- Increased tumor size and weight in stressed mice.
- Higher levels of myeloid cells within tumors.
- Increased TAM infiltration in the tumor microenvironment.
A Call for Comprehensive Care: Addressing Mental Health in Prostate Cancer
The research findings emphasize the importance of treating the whole person—including mental health—when addressing cancer. Integrating mental health care into standard cancer treatment may lead to better outcomes. These advances offer hope for improved prostate cancer treatment strategies, potentially enhancing the quality of life and survival rates for countless men. As science continues to explore the intricate connection between the mind and body, the need for comprehensive, patient-centered care becomes increasingly clear.
