Decompressive Craniectomy: Understanding Hydrocephalus Risk
"A Guide to Identifying and Managing Post-Traumatic Hydrocephalus after Skull Removal Surgery"
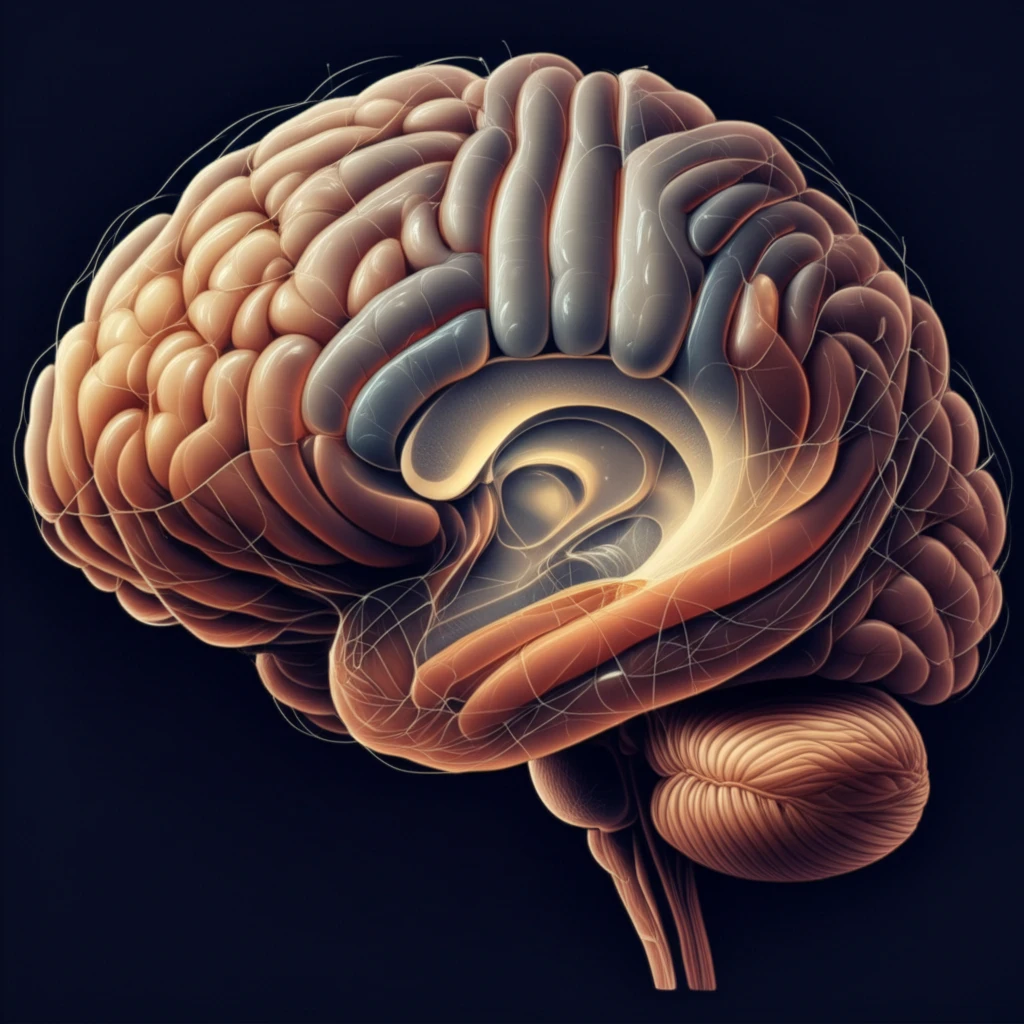
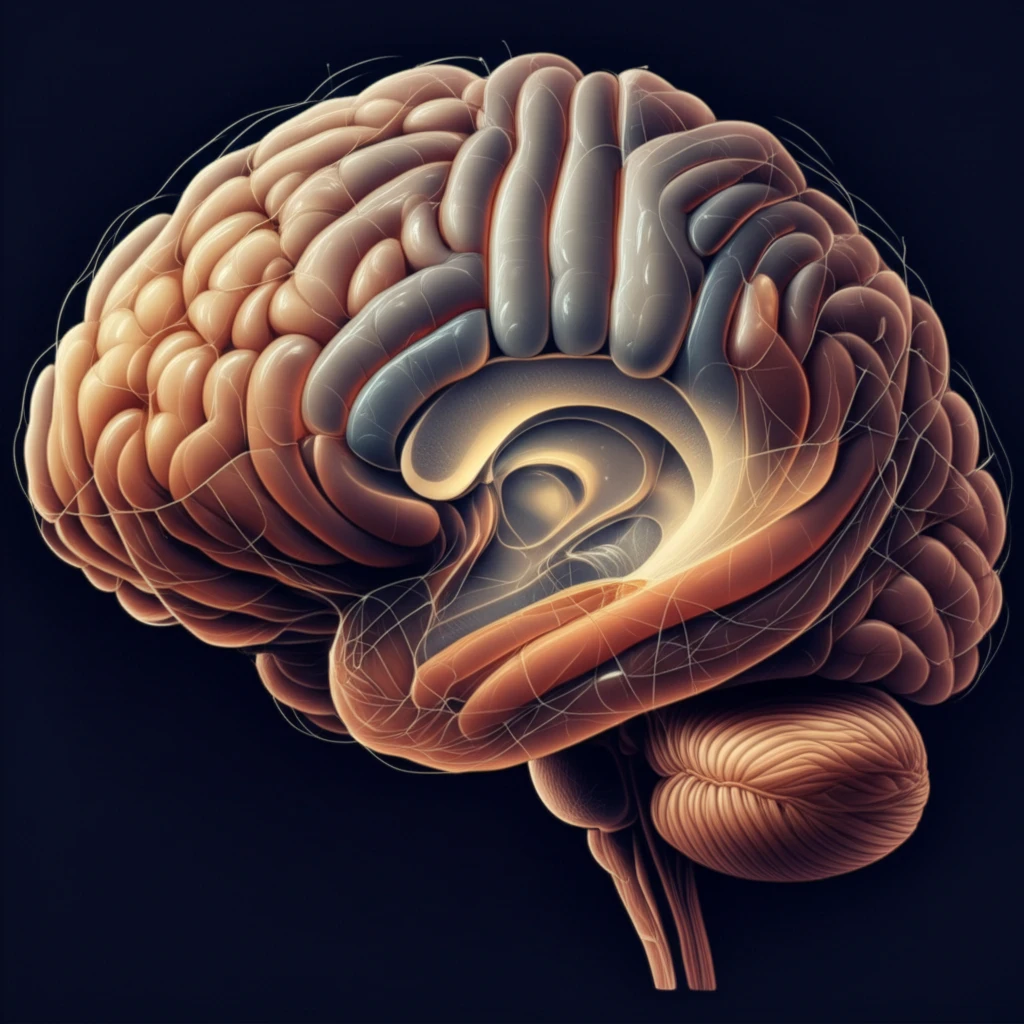
Decompressive craniectomy is a procedure neurosurgeons use to treat elevated pressure inside the skull when other methods aren't effective. It involves removing a portion of the skull to allow the brain to swell without being compressed. While this surgery can be life-saving, it's also associated with potential complications.
One such complication is post-traumatic hydrocephalus (PTH), a condition where there's an abnormal buildup of cerebrospinal fluid (CSF) in the brain's ventricles. This can lead to increased pressure and neurological problems. Understanding the risk factors for PTH after decompressive craniectomy is crucial for early detection and management.
This article breaks down recent research into identifying those risk factors, particularly focusing on the connection between hydrocephalus and subdural hygroma (SDG), a collection of fluid between the brain's surface and the dura mater, following decompressive craniectomy. Knowing these risks can help doctors monitor patients more closely and intervene when necessary.
Unveiling the Risks: What Increases Hydrocephalus After Craniectomy?
A recent study investigated the incidence and risk factors for post-traumatic hydrocephalus (PTH) following decompressive craniectomy (DC). The study focused on 94 patients with severe head injuries requiring DC, with a closer analysis of 41 patients who had at least four follow-up CT scans over three months. Post-traumatic hydrocephalus was identified using specific measurements on CT scans (frontal horn index) and clinical symptoms. Subdural hygroma (SDG) was defined as a low-density area greater than 5mm thick on CT scans.
- Hydrocephalus developed in 29.3% of patients.
- Subdural hygroma (SDG) occurred in 48.8% of patients.
- A significant association was found between the development of PTH and delayed cranioplasty (skull reconstruction).
- Interhemispheric SDG (SDG located between the brain hemispheres) was also significantly associated with PTH.
- No significant relationship was found between PTH and factors like age, sex, initial Glasgow Coma Scale (GCS) score, or the presence of certain types of bleeding.
Key Takeaways: What This Means for Patients and Caregivers
This research highlights the importance of being aware of the potential for hydrocephalus to develop after decompressive craniectomy. While the surgery is often necessary to save lives and reduce brain pressure, it's crucial to monitor patients closely for signs of complications.
The study emphasizes that delayed skull reconstruction and the presence of interhemispheric subdural hygroma increase the risk of developing hydrocephalus. This knowledge can help doctors make informed decisions about the timing of cranioplasty and the need for closer monitoring in patients with interhemispheric SDG.
If you or a loved one has undergone decompressive craniectomy, it's essential to discuss these findings with your medical team. Early detection and management of hydrocephalus can significantly improve outcomes and quality of life.
