Decoding Thalassemia: Understanding Red Cell Alloimmunization and the Importance of Blood Transfusions
"A Comprehensive Guide to Alloimmunization in Thalassemia Patients: What It Is, Why It Happens, and How It's Managed"
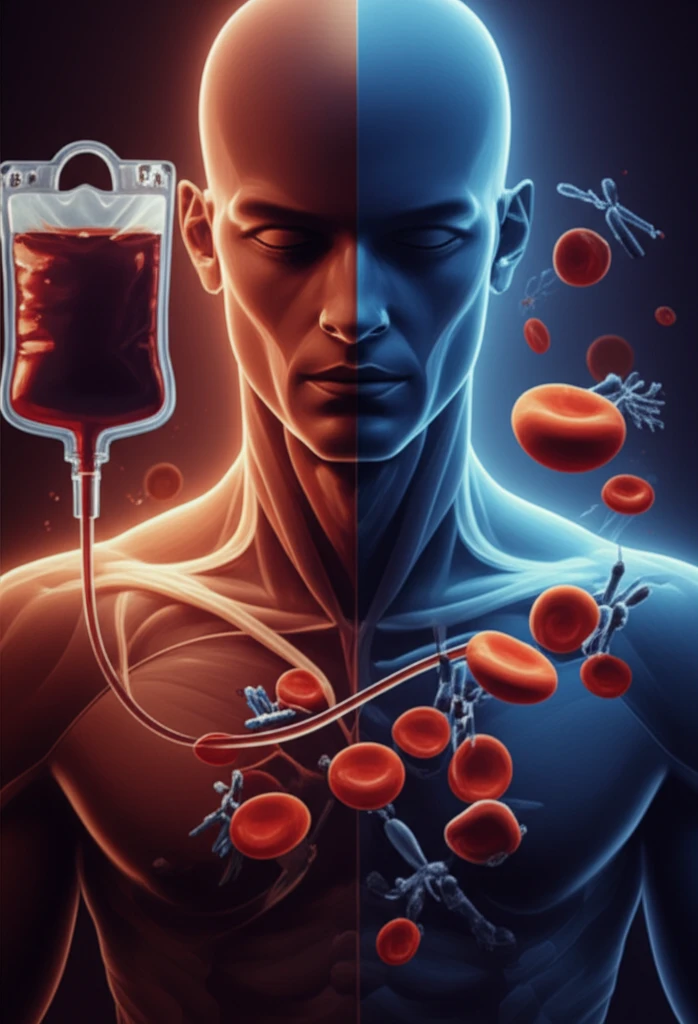
Thalassemia represents a group of inherited blood disorders characterized by defects in hemoglobin production, leading to anemia. For individuals with severe forms of thalassemia, regular red blood cell transfusions become a critical part of their care. These transfusions help manage anemia and improve overall quality of life.
However, frequent transfusions can lead to a concerning complication: red cell alloimmunization. This occurs when the recipient's immune system recognizes the transfused red blood cells as foreign and starts producing antibodies against them. These antibodies can target specific antigens on the surface of the red blood cells, potentially leading to a range of clinical problems.
Understanding alloimmunization is crucial for thalassemia patients, their families, and healthcare providers. Early detection and proper management can significantly reduce the risks associated with this condition. This article explores the complexities of alloimmunization in thalassemia, shedding light on why it happens, how it's detected, and what steps can be taken to mitigate its impact.
What is Red Cell Alloimmunization in Thalassemia?
Alloimmunization is an immune response where the body produces antibodies against foreign red blood cell antigens. In thalassemia patients who receive frequent blood transfusions, the risk of alloimmunization increases because they are exposed to a variety of red blood cell antigens from different donors.
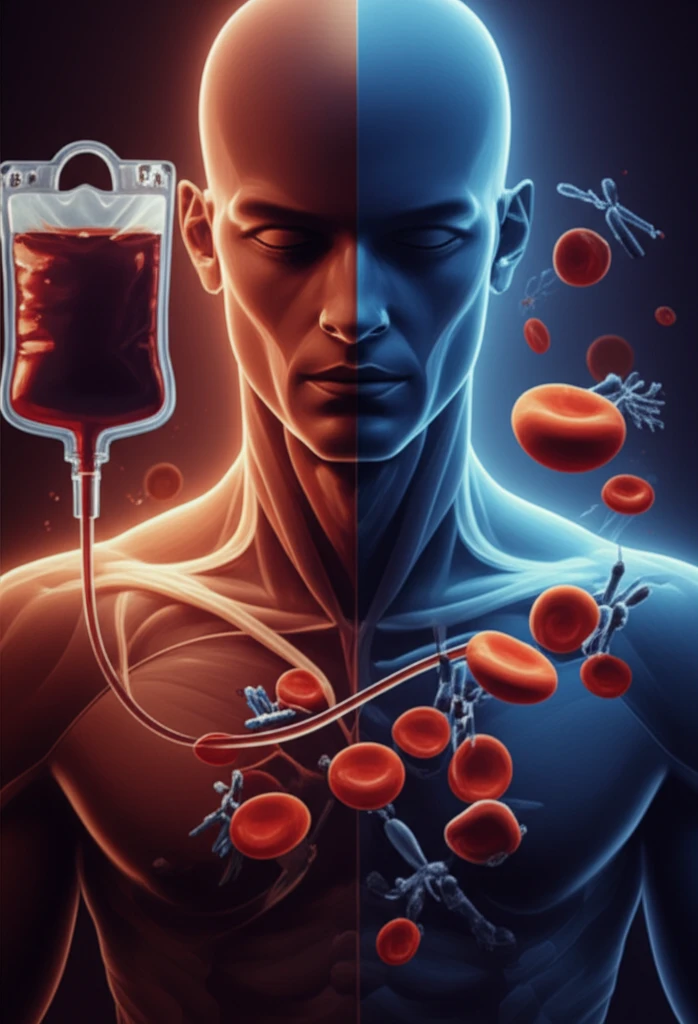
- Delayed Hemolytic Transfusion Reactions: The alloantibodies attack the transfused red cells, leading to their premature destruction.
- Increased Transfusion Requirements: As the transfused cells are destroyed more quickly, the patient may need more frequent transfusions to maintain adequate hemoglobin levels.
- Difficulty in Cross-Matching Blood: The presence of multiple alloantibodies can make it difficult to find compatible blood for future transfusions.
- Increased Risk of Morbidity: Severe alloimmunization can contribute to overall health issues and complications.
The Path Forward: Improving Transfusion Strategies
Managing alloimmunization in thalassemia patients is an ongoing challenge. By using advanced detection methods, tailoring transfusion strategies, and exploring novel therapies, healthcare professionals can minimize the impact of alloimmunization and improve the long-term outcomes for individuals living with thalassemia. Continuous research and collaboration are essential to ensure a brighter, healthier future for these patients.
