Decoding Prostate Cancer: How MRI Scans and Gleason Scores Are Changing the Game
"Learn how cutting-edge MRI technology and Gleason scores are teaming up to revolutionize prostate cancer diagnosis and treatment, offering new hope for personalized care."
Prostate cancer stands as a significant health challenge, being one of the most prevalent cancers among men and a leading cause of cancer-related deaths in industrialized nations. What makes prostate cancer particularly complex is its heterogeneous nature; it can range from a slow-growing, indolent condition to a highly aggressive and life-threatening disease. This variability underscores the critical need for accurate methods to classify the aggressiveness of the cancer, ensuring that each patient receives the most appropriate and effective treatment strategy.
The ultimate goal in managing prostate cancer is to strike a delicate balance: identifying and aggressively treating those patients who stand to benefit most from radical therapies, while simultaneously avoiding overtreatment in individuals where the cancer poses little threat to their overall health. Traditional methods of assessing prostate cancer aggressiveness have limitations. While significant progress has been made in characterizing the disease, there remains a need for reliable, non-invasive tools to accurately gauge how aggressive a particular cancer may be.
One of the established methods for predicting prostate cancer aggressiveness is the pathological Gleason score (GS). The GS is determined through a biopsy, where tissue samples are taken and examined under a microscope. The biopsy results are then translated into a GS, which indicates the tumor's characteristics. A higher GS typically suggests a more aggressive cancer, influencing treatment decisions. However, this method isn't without its drawbacks. The invasive nature of biopsies, potential for sampling errors, and the risk of adverse events highlight the need for complementary diagnostic approaches.
MRI and Gleason Score: A Powerful Partnership
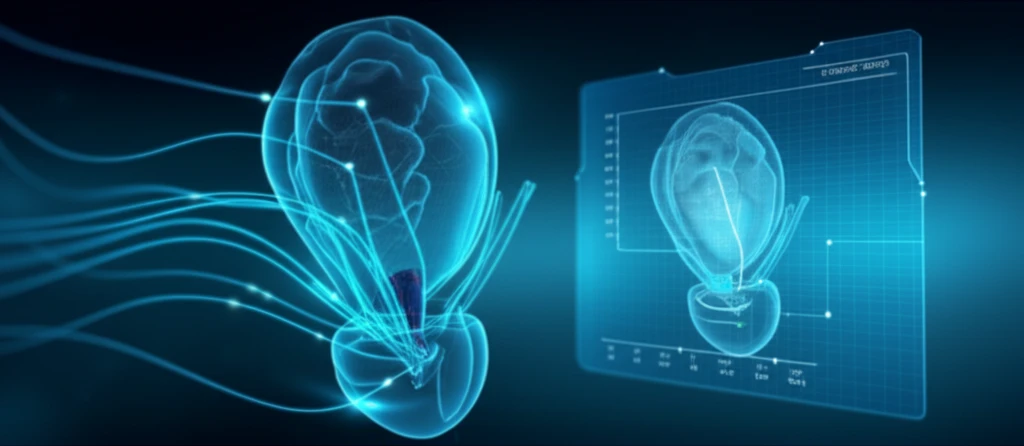
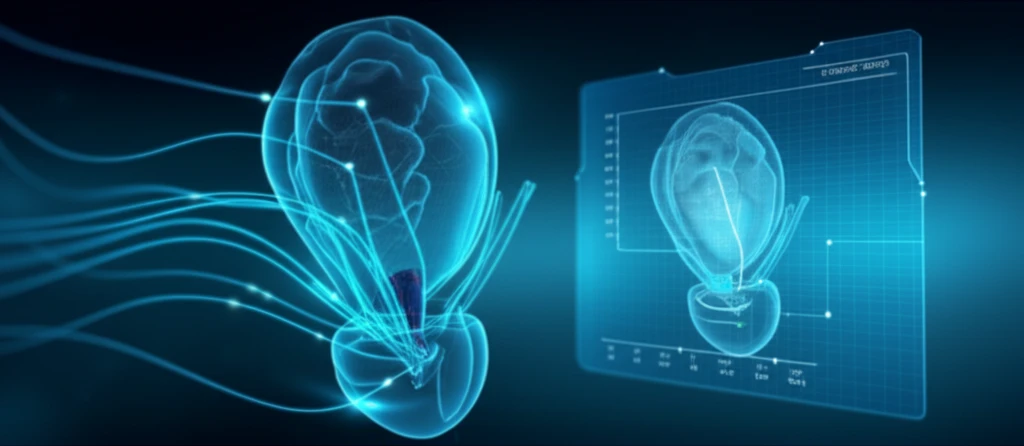
Recent advancements in medical imaging have brought multiparametric magnetic resonance imaging (mpMRI) to the forefront of prostate cancer diagnostics. This advanced imaging technique includes diffusion-weighted imaging (DWI), which provides valuable insights into the characteristics of prostate tumors. The apparent diffusion coefficient (ADC) value, derived from DWI sequences, has emerged as a novel tool for enhancing the diagnosis and management of prostate cancer.
- Improved Diagnosis: ADC values provide critical information about tumor characteristics that guide diagnosis.
- Treatment Planning: These values help doctors tailor treatment plans based on the aggressiveness of the cancer.
- Non-Invasive Assessment: ADC values are obtained through non-invasive MRI, reducing the need for repeated biopsies.
The Future of Prostate Cancer Diagnosis
The study's findings suggest that GS can be predicted by ADC values for tumor lesions on DWI. Furthermore, a cutoff ADC value may be useful for distinguishing GS 6 prostate cancer from prostate cancer with a GS of at least 7. By integrating advanced imaging techniques like mpMRI with established diagnostic tools like the Gleason score, healthcare professionals can move towards more personalized and effective strategies in the fight against prostate cancer.
