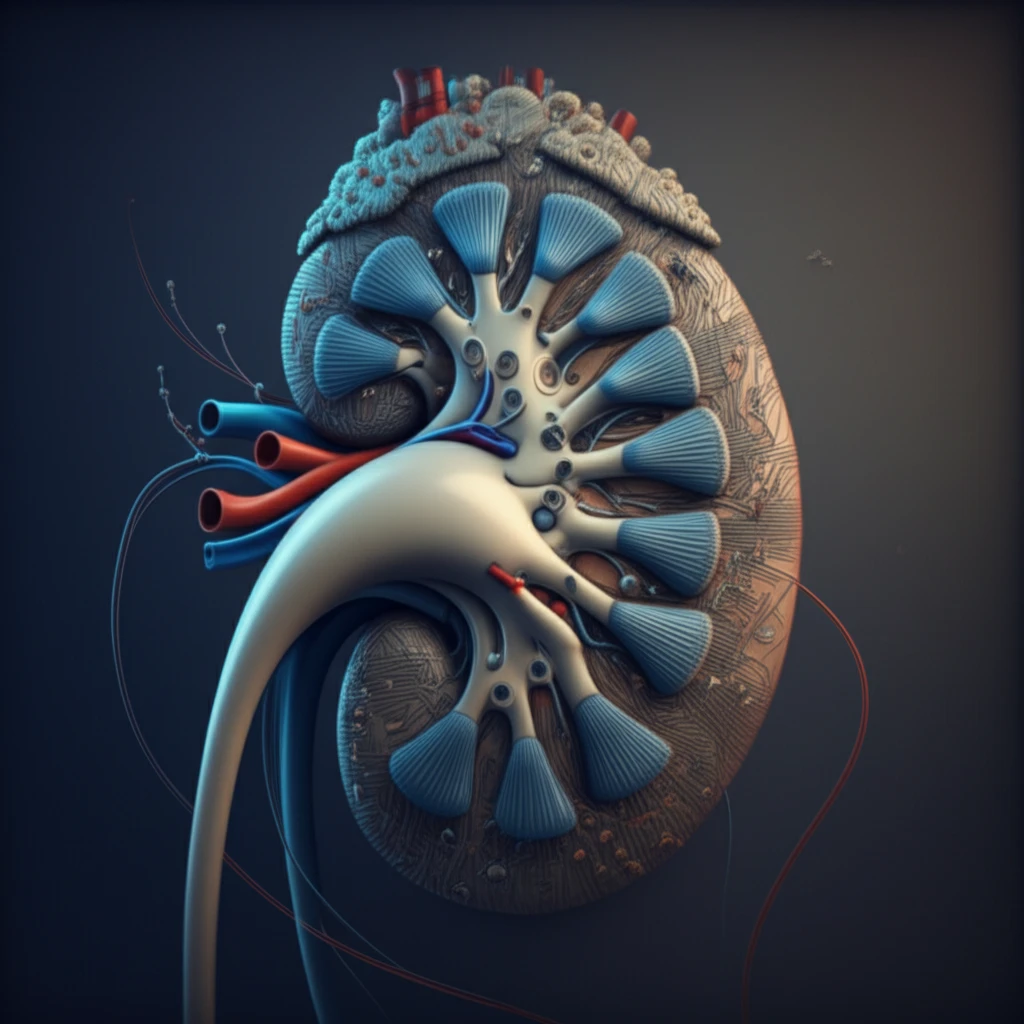
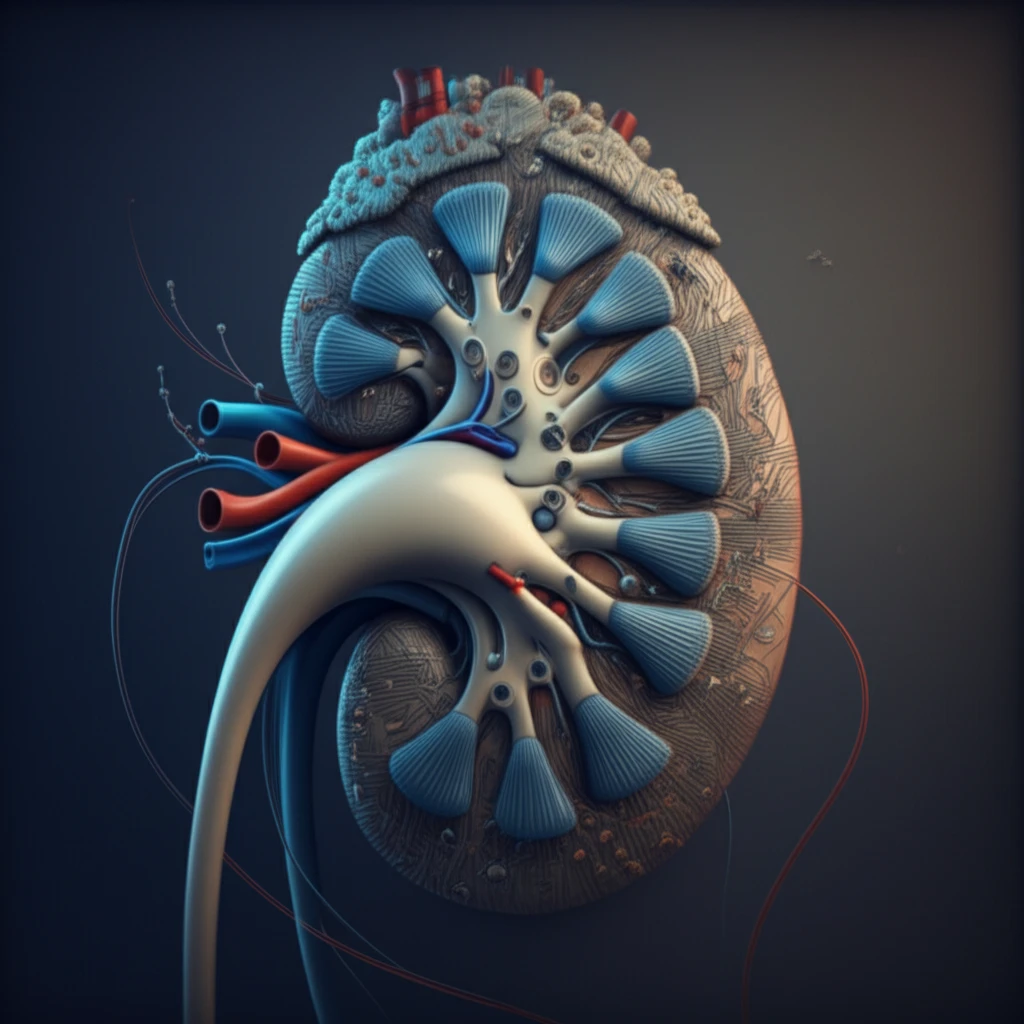
Decoding Kidney Health: What Critical Illness Studies Reveal
"A systematic review uncovers how acute renal dysfunction is defined and included in major clinical trials, impacting patient outcomes."
In the landscape of evidence-based medicine, multicenter, prospective, randomized controlled trials (RCTs) stand as the gold standard for evaluating treatment benefits and ensuring the effectiveness of interventions. Patient-centered outcomes, such as mortality, are frequently the preferred metrics. However, even with agreements on classifying renal dysfunction in critically ill patients, questions remain about how consistently new classification systems are applied in RCTs.
Acute renal dysfunction, affecting a substantial portion of hospitalized patients and those in intensive care units (ICUs), is not just a complication; it's an independent risk factor for mortality. It also leads to prolonged hospital stays and increased healthcare costs.
To shed light on these issues, a systematic review was conducted to assess the definition and inclusion of renal dysfunction in multicenter RCTs involving critically ill patients, with mortality as a primary endpoint. The study also evaluates criteria for determining the severity and progression of kidney injury, providing valuable insights for both clinicians and researchers.
How is Kidney Dysfunction Defined in Critical Care Trials?
The review analyzed 46 multicenter RCTs that included mortality as a primary outcome. These trials studied a wide range of critical conditions, including sepsis, acute respiratory distress syndrome, and shock. Interventions varied from drug treatments to mechanical ventilation strategies.
- Inclusion of Renal Data: A significant majority (78.3%) of trial reports provided information on renal function.
- Infrequent Use of Standardized Criteria: Only a small fraction (15.2%) reported mean or median serum creatinine levels or glomerular filtration rates (eGFRs).
- SOFA Score Dominance: The Sequential Organ Failure Assessment (SOFA) score was the most common definition of renal dysfunction (43.5%).
- Limited Adoption of RIFLE/AKIN/KDIGO: RIFLE, AKIN, and KDIGO criteria were used in only 10.9% of trials.
- Missing Criteria: A notable percentage (28.3%) of trials did not report any specific criteria for defining acute renal dysfunction.
Implications for Clinical Practice and Research
The inconsistent use of standardized definitions for acute renal dysfunction in critical care RCTs raises questions about the application of evidence-based guidelines in clinical practice. While the SOFA score is frequently used, the underutilization of RIFLE, AKIN, and KDIGO criteria suggests a gap in adopting newer classification systems.
A unified approach to defining acute renal dysfunction is essential for clinical practice, research, and public health. This standardization would improve the consistency and comparability of trial results, leading to better-informed clinical decisions.
Future research should focus on evaluating the validity and identifying the barriers to the utilization of different scoring systems, ultimately improving patient care in critical illness.
