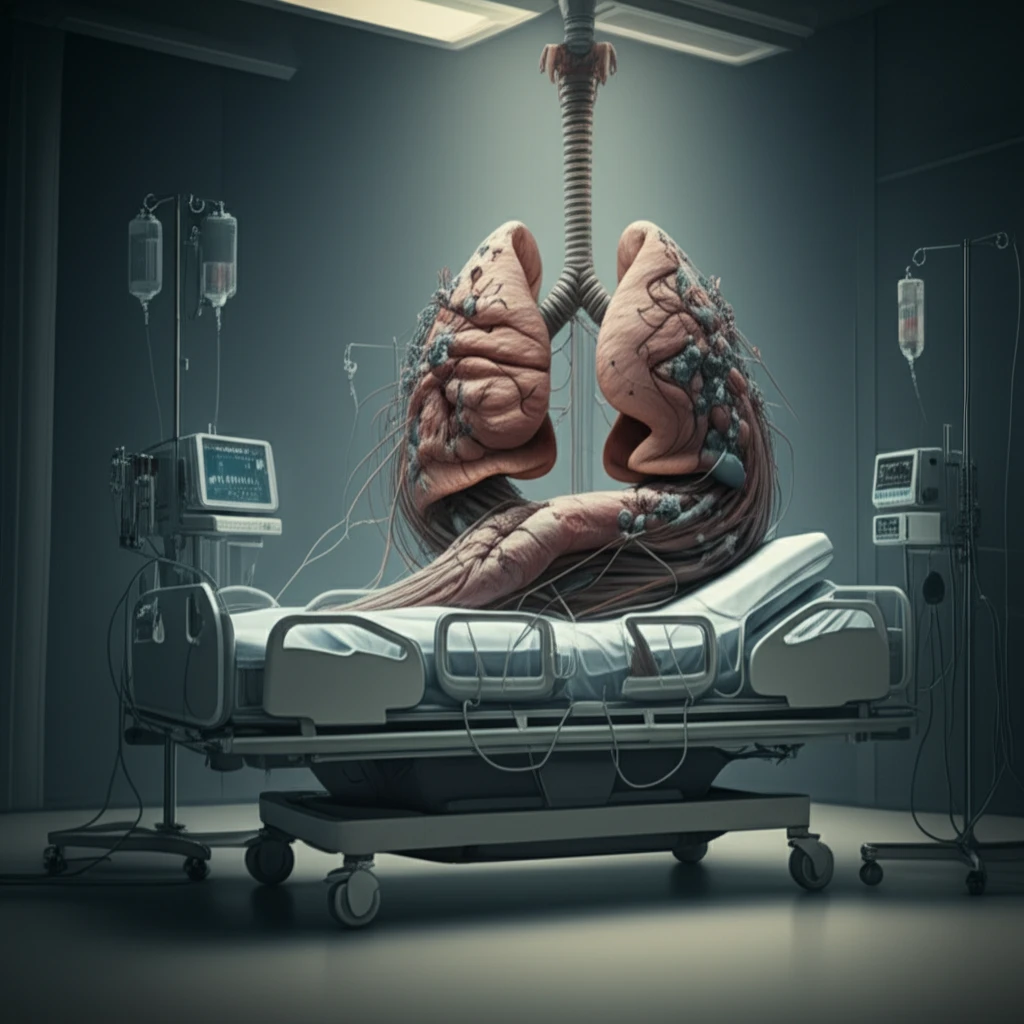
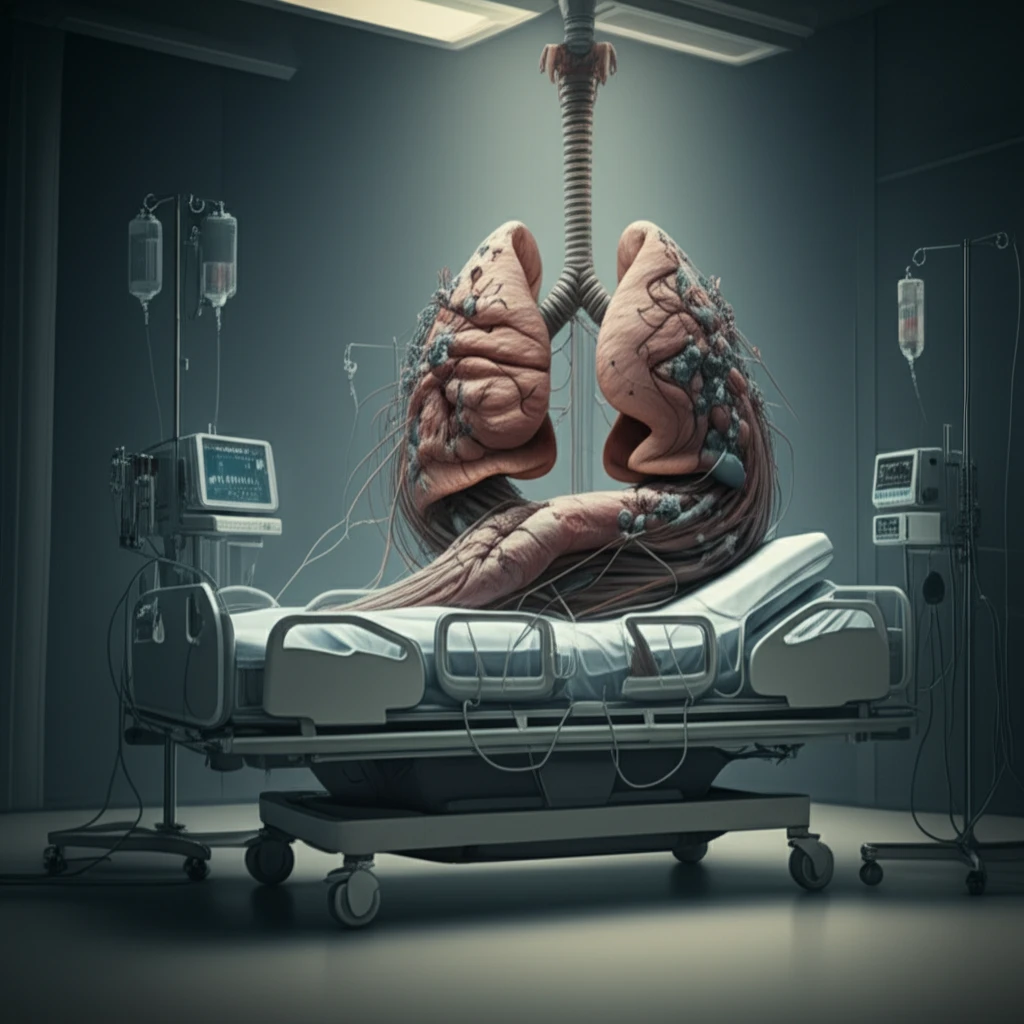
Decoding ICU Risks: How to Improve Survival Rates for Interstitial Lung Disease Patients
"A deep dive into the factors influencing mortality in the intensive care unit (ICU) for individuals battling interstitial lung disease (ILD). Understand the key risk factors and discover how targeted interventions can improve outcomes."
Interstitial lung diseases (ILDs) are a complex group of over 200 different conditions characterized by inflammation and scarring in the lungs. This damage makes it difficult to breathe and can lead to substantial morbidity and mortality. When ILD patients experience acute respiratory problems, they often require admission to the intensive care unit (ICU).
However, outcomes for ILD patients in the ICU have historically been poor, complicated by the diverse nature of ILDs and evolving diagnostic criteria. This heterogeneity makes it challenging for doctors to provide accurate prognoses and tailor treatments effectively. Identifying the specific factors that increase mortality risk is crucial for improving patient care.
This article explores the key risk factors associated with mortality and mortality rates in ILD patients within the ICU setting. We'll delve into the findings of a systematic review analyzing multiple studies to identify critical variables that impact survival. The aim is to provide patients and their families with a clearer understanding of the challenges, as well as to inform healthcare professionals about strategies to optimize outcomes.
Key Risk Factors Affecting ILD Mortality in the ICU
A comprehensive review of medical literature was conducted, examining numerous studies focused on ILD patients admitted to the ICU. The analysis aimed to pinpoint factors consistently linked to higher mortality rates. The review differentiated between studies focusing on mixed-ILD populations (various ILD types) and those specifically examining idiopathic pulmonary fibrosis (IPF), a particularly aggressive form of ILD.
- Elevated APACHE Score: The Acute Physiology and Chronic Health Evaluation (APACHE) score is a general indicator of disease severity. Higher APACHE scores in ILD patients strongly correlated with increased mortality. This indicates that overall illness severity significantly impacts survival.
- Hypoxemia: Low levels of oxygen in the blood (hypoxemia) were consistently associated with poorer outcomes. Adequate oxygenation is crucial for these patients, and difficulties in maintaining sufficient oxygen levels signal a higher risk.
- Mechanical Ventilation: The need for mechanical ventilation, especially invasive ventilation, was a major predictor of mortality. While sometimes necessary to support breathing, mechanical ventilation can also introduce complications.
Improving Survival: What Does This Mean for ILD Patients and Their Families?
While the findings highlight the serious challenges faced by ILD patients in the ICU, they also offer valuable insights for improving care. Recognizing the significant impact of factors like APACHE scores and hypoxemia allows medical teams to focus on aggressive management of overall illness severity and oxygenation.
The observation that mortality rates may be declining since the 1990s suggests progress in treatment approaches. Continued research into ventilation strategies, such as minimizing high PEEP (positive end-expiratory pressure) and exploring non-invasive ventilation options, holds promise for better outcomes.
It's important to remember that this research represents a broad overview. Individual patient outcomes will vary depending on the specific type of ILD, the stage of the disease, and overall health. Open communication with your medical team is crucial for understanding your individual risk factors and making informed decisions about treatment.
