Decoding Huntington's: How Heart Health Holds the Key to a Devastating Disease
"New research unveils the surprising link between Huntington's disease and heart problems, offering hope for earlier detection and better treatments."
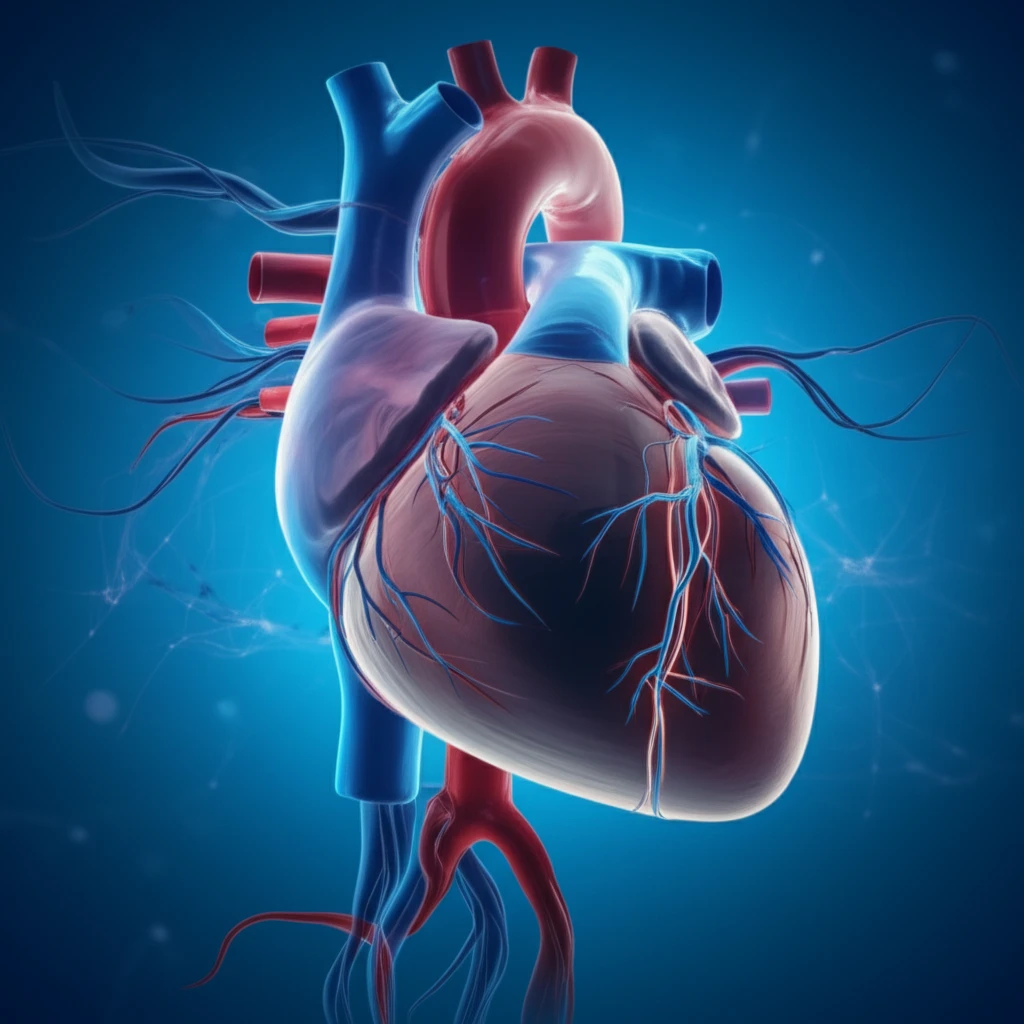
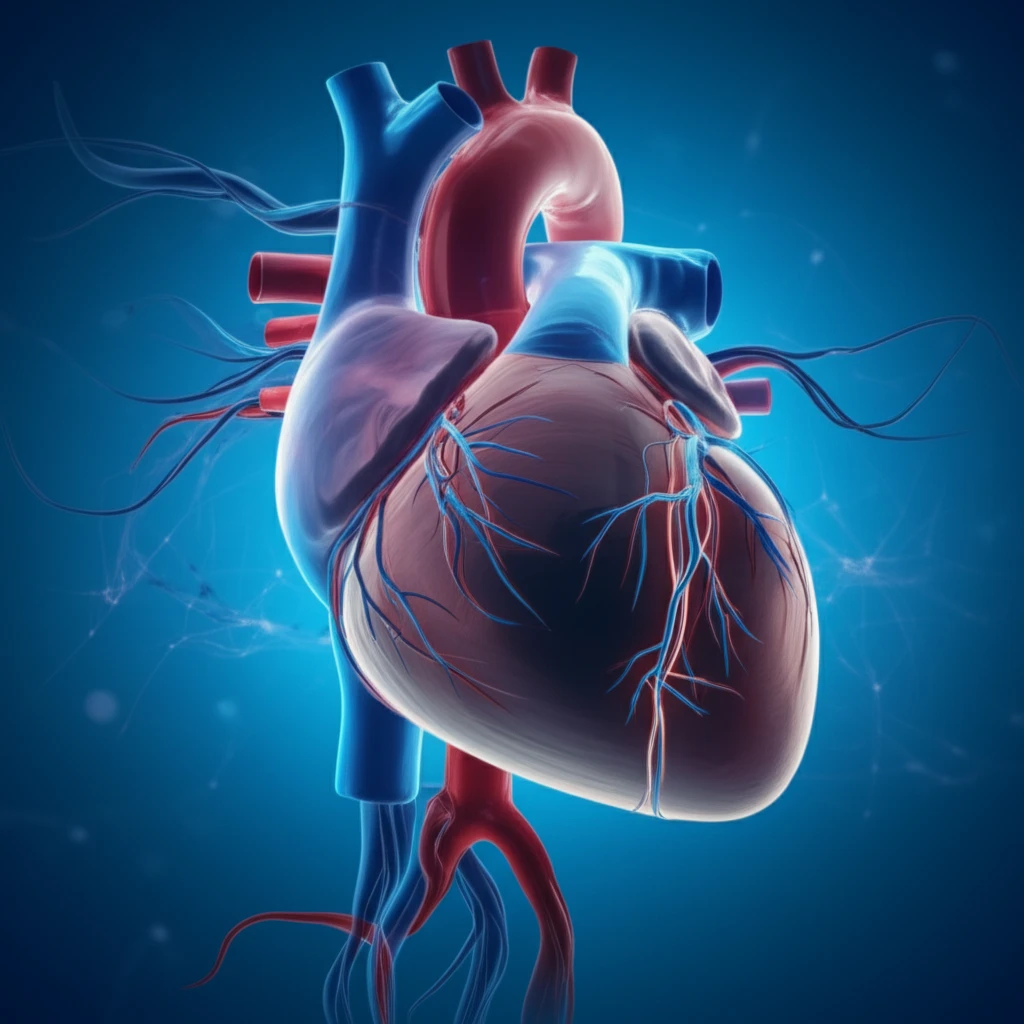
Huntington's disease (HD) has long been recognized as a devastating neurodegenerative disorder, primarily affecting movement, cognition, and mental well-being. While the focus has traditionally been on the brain, emerging evidence reveals a significant connection between HD and cardiovascular health. This connection suggests that heart-related problems are not merely a complication of HD, but an integral part of the disease's progression.
Cardiovascular issues are a major cause of death in individuals with HD, highlighting the urgent need to understand how this disease impacts the heart. Relatively little is known about the specific ways HD affects the peripheral systems, including the heart. Understanding these connections could lead to earlier diagnosis and more effective treatment strategies.
Recent research has begun to unravel the complexities of cardiac dysfunction in HD. By using a range of advanced techniques, scientists are exploring the electro-mechanical properties of the heart in a mouse model of HD, seeking to identify the underlying mechanisms that contribute to heart problems in HD patients. This article explores their findings and what they mean for the future of HD treatment.
Unraveling the Heart-HD Connection: Key Research Findings
The research team employed various methods to assess cardiac function in both in-vivo (living organisms) and in-vitro (laboratory) settings. They used a well-characterized mouse model of HD known as BACHD, which exhibits several key features of the human disease. These experiments revealed several significant cardiac abnormalities in the HD model:
- ECG Abnormalities: The BACHD mice showed clear signs of conduction disturbances, including prolonged QT intervals (a measure of the heart's electrical recovery time) and ST-segment deviations, both indicative of cardiac dysfunction.
- Cellular-Level Defects: Cardiomyocytes (heart muscle cells) isolated from the BACHD mice exhibited abnormal electrical and mechanical behavior. This included prolonged action potentials (the electrical signals that trigger heartbeats), erratic contractions, and impaired relaxation.
- Calcium Imbalance: The researchers found an increase in calcium waves and elevated activity of CaMKII (a calcium-dependent enzyme), suggesting that HD disrupts the delicate balance of calcium within heart cells. Calcium plays a crucial role in muscle contraction and relaxation, so imbalances can lead to arrhythmias and other cardiac problems.
- Mitochondrial Damage: The team observed structural abnormalities in the mitochondria of BACHD-derived cardiomyocytes, indicating increased oxidative stress. Oxidative stress occurs when there's an imbalance between the production of harmful free radicals and the body's ability to neutralize them.
- Antioxidant Imbalance: Consistent with the mitochondrial damage, the study detected imbalances in the activity of superoxide dismutase and glutathione peroxidase, two key antioxidant enzymes that protect cells from oxidative damage.
What This Means for Huntington's Disease Patients
This research offers valuable insights into the link between Huntington's disease and heart health, which may lead to earlier detection and better treatments. The identification of specific cardiac abnormalities in HD could pave the way for developing targeted therapies to protect the heart and improve the overall quality of life for individuals living with this challenging condition.
The study highlights the importance of considering heart health as an integral part of managing Huntington's disease. Regular cardiac screenings and proactive interventions may help to mitigate the risk of heart-related complications and improve patient outcomes.
While more research is needed, these findings represent a significant step forward in understanding the complexities of Huntington's disease and offer hope for a future where the disease can be managed more effectively, addressing both the neurological and cardiovascular aspects of the condition.
