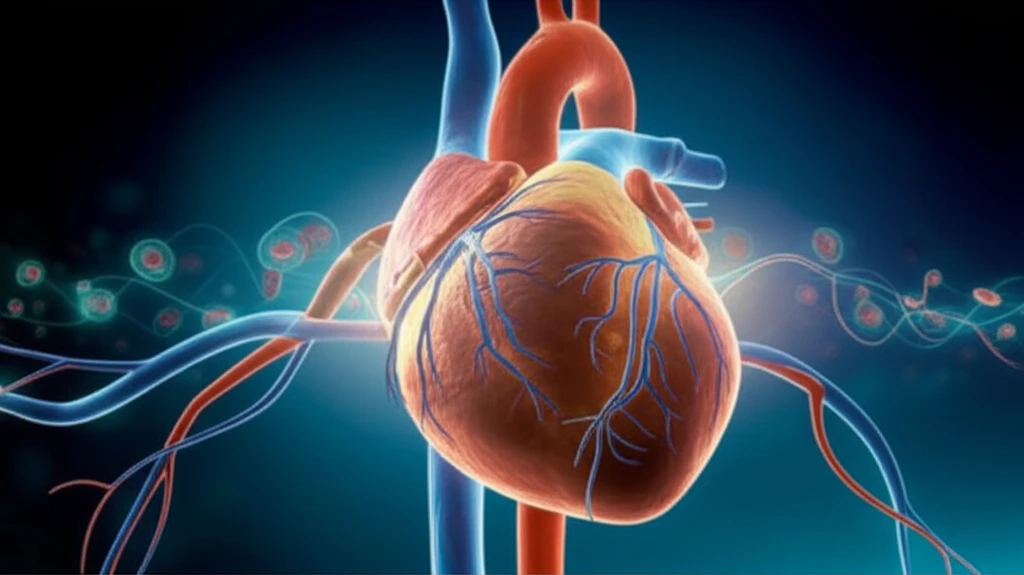
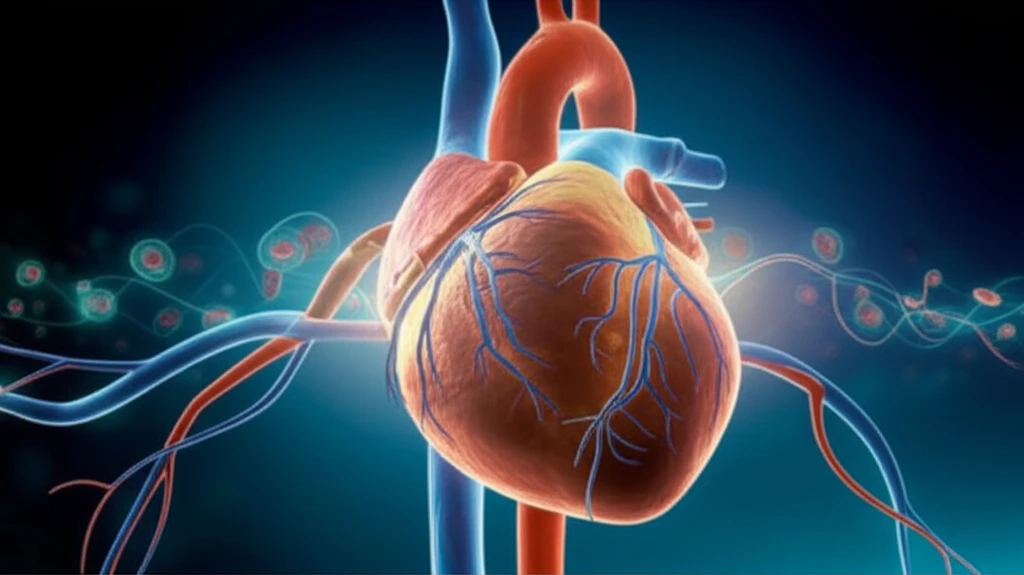
Decoding Heart Failure: How Atrial Fibrillation and Stem Cell Therapy are Changing the Game
"New insights into diagnosing heart failure in dyspneic patients and the potential of stem cell therapy for chronic heart conditions."
Heart failure remains a significant global health challenge, affecting millions worldwide. As medical science advances, new research emerges that refines our understanding and treatment of this complex condition. Recent studies have shed light on the intricate relationship between atrial fibrillation (AF) and heart failure diagnosis, as well as the potential of stem cell therapy to improve outcomes for those with chronic heart failure.
This article delves into two pivotal research areas: the influence of atrial fibrillation on the accuracy of NT-proBNP (N-terminal pro-brain natriuretic peptide) in diagnosing acute heart failure, and the therapeutic potential of stem cell therapy for chronic heart failure patients. By examining these findings, we aim to provide a comprehensive overview of how these advancements could reshape the landscape of heart failure management.
Whether you're a healthcare professional, a patient, or simply interested in the latest medical breakthroughs, this article offers valuable insights into the evolving strategies for diagnosing and treating heart failure. Join us as we explore these cutting-edge developments and their potential impact on patient care.
The Atrial Fibrillation Connection: How AF Impacts Heart Failure Diagnosis
Diagnosing acute heart failure (AHF) in patients experiencing dyspnea (shortness of breath) can be challenging. N-terminal pro-brain natriuretic peptide (NT-proBNP) is a widely used biomarker in this process, but its accuracy can be affected by various factors, including the presence of atrial fibrillation. A recent study aimed to investigate the influence of AF on NT-proBNP levels in dyspneic patients suspected of having AHF.
- Elevated NT-proBNP Levels: Patients with AF had significantly higher NT-proBNP levels compared to those without AF (4482.0 pg/ml vs 1302.0 pg/ml, P = 0.000).
- AF in AHF Patients: A significant proportion (46.9%) of patients diagnosed with AHF also had AF.
- No Difference in AHF Group: No significant difference in NT-proBNP levels was observed between AHF patients with and without AF.
- Impact in Non-AHF Group: NT-proBNP concentrations were significantly higher in non-AHF patients with AF compared to those without AF.
- Reduced Diagnostic Accuracy: The diagnostic accuracy of NT-proBNP for AHF was lower in patients with AF [AUC: 0.759, 95%CI (0.677-0.841) vs 0.931, 95% CI (0.903-0.985), P < 0.050].
- Optimal Cut-off Points: The optimal NT-proBNP cut-off point for diagnosing AHF was 3700 pg/ml in AF patients (74% sensitivity, 65% specificity) and 1900 pg/ml in non-AF patients (91% sensitivity, 79% specificity).
The Future of Heart Failure Treatment
The ongoing research into heart failure continues to offer new hope for patients worldwide. By understanding the complexities of conditions like atrial fibrillation and harnessing the potential of innovative therapies like stem cell therapy, we can pave the way for more effective, personalized treatments. Stay informed, stay proactive, and work closely with your healthcare providers to navigate the evolving landscape of heart failure care.
