Decoding Gonorrhea: How a Clever Protein Helps It Evade Your Immune System
"Scientists uncover the sneaky tactics of the NspA protein in gonorrhea, revealing potential new targets for vaccines and treatments."
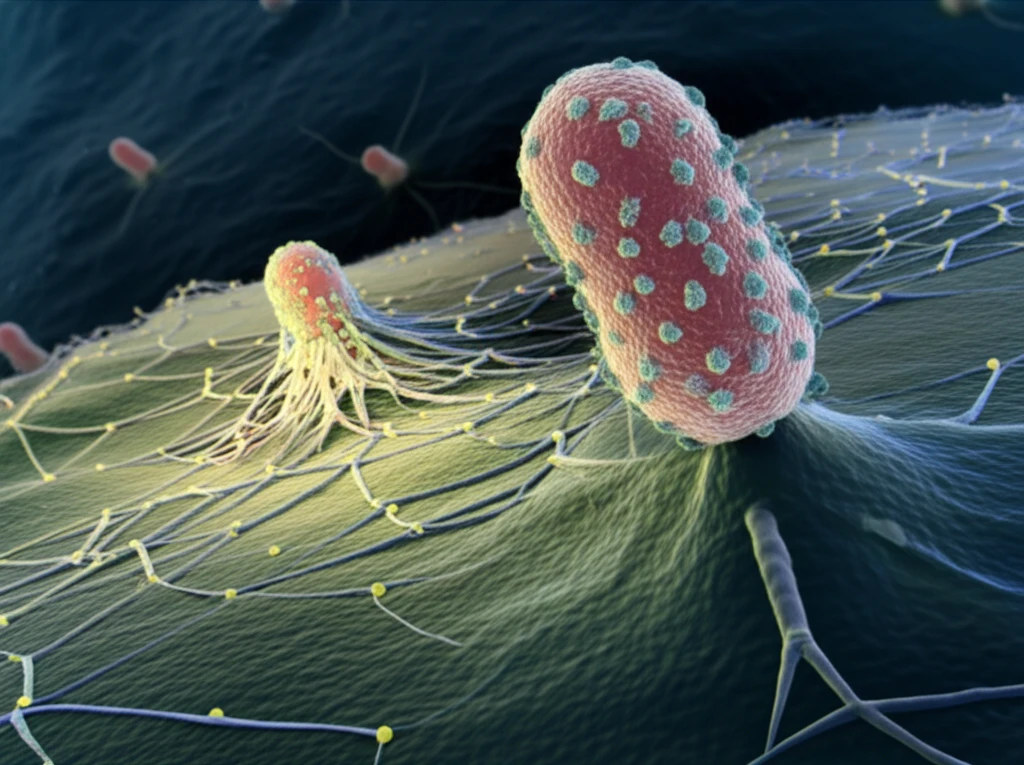
Gonorrhea, a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae (Ng), affects millions globally each year. The rise of antibiotic-resistant strains has made it crucial to understand how this bacterium evades the immune system. New research sheds light on a key player in this evasion: the Neisserial surface protein A (NspA).
Scientists have long known that Ng has several tricks to avoid being destroyed by the complement system, a part of the immune system that directly attacks bacteria. One of these tricks involves binding to Factor H (FH), a protein that regulates and inhibits the complement system, preventing it from harming the body's own cells. This research delves into how NspA contributes to FH binding and, ultimately, to the bacterium's survival.
This article explores the recent findings about NspA's role in gonorrhea, comparing its function to that of its counterpart in Neisseria meningitidis (Nm), a bacterium that causes meningitis. Understanding these mechanisms is vital for developing effective vaccines and therapies against this global health threat.
NspA: The Master of Disguise in Gonorrhea's Immune Evasion
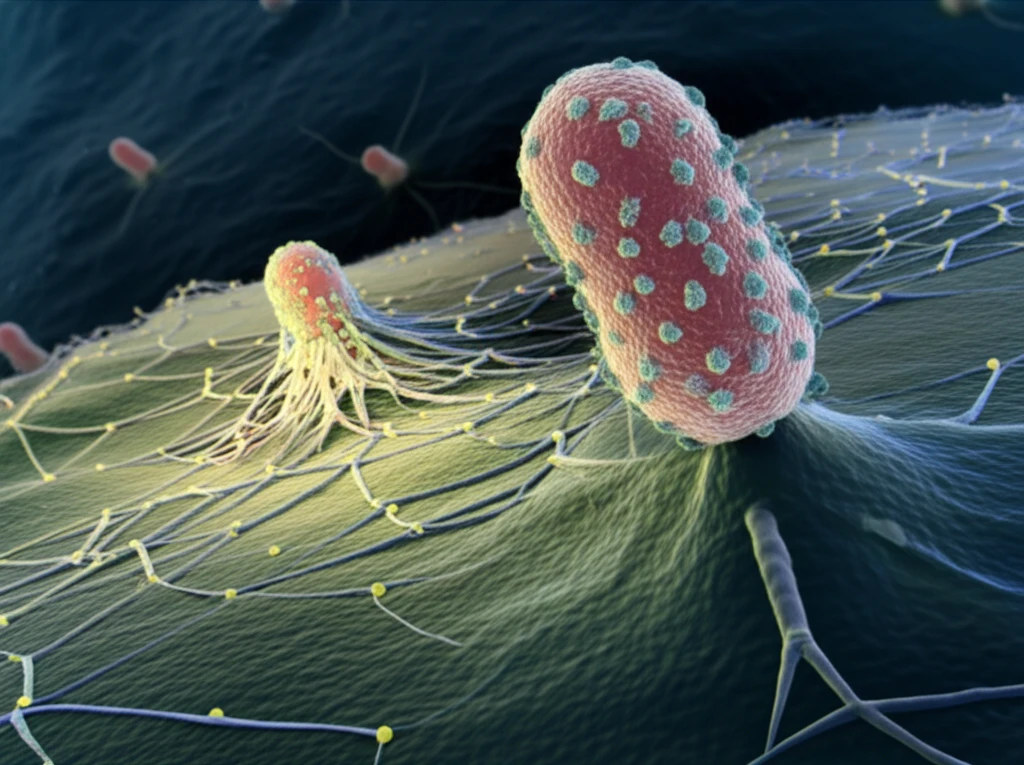
The study pinpoints NspA as a critical factor in Ng's ability to resist the body's natural defenses. NspA, located on the surface of the bacterium, directly interacts with Factor H (FH) and Factor H-like protein 1 (FHL-1), both key inhibitors of the complement system. By binding to these proteins, NspA essentially tells the immune system to back off, allowing the gonorrhea bacteria to thrive.
- Direct Interaction: NspA binds directly to FH and FHL-1, disrupting the complement cascade.
- LOS Independence: NspA's function doesn't rely on LOS sialylation, marking it as a distinct evasion strategy.
- FH Domains 6 and 7: Binding occurs specifically through FH domains 6 and 7, crucial regions for complement regulation.
Future Directions: Targeting NspA for New Therapies
The detailed understanding of NspA's role in gonorrhea's immune evasion opens new doors for therapeutic intervention. By identifying the specific regions of NspA that interact with FH, scientists can design targeted vaccines and immunotherapies. These strategies could block NspA's ability to bind to FH, allowing the immune system to effectively clear the infection.
