Decoding Digestive Distress: A Guide to Understanding and Improving Timing in ERCP and Cholecystectomy
"Learn how the timing of these procedures can significantly impact your recovery and overall well-being. Explore the latest research and expert insights to navigate the complexities of biliary obstruction."
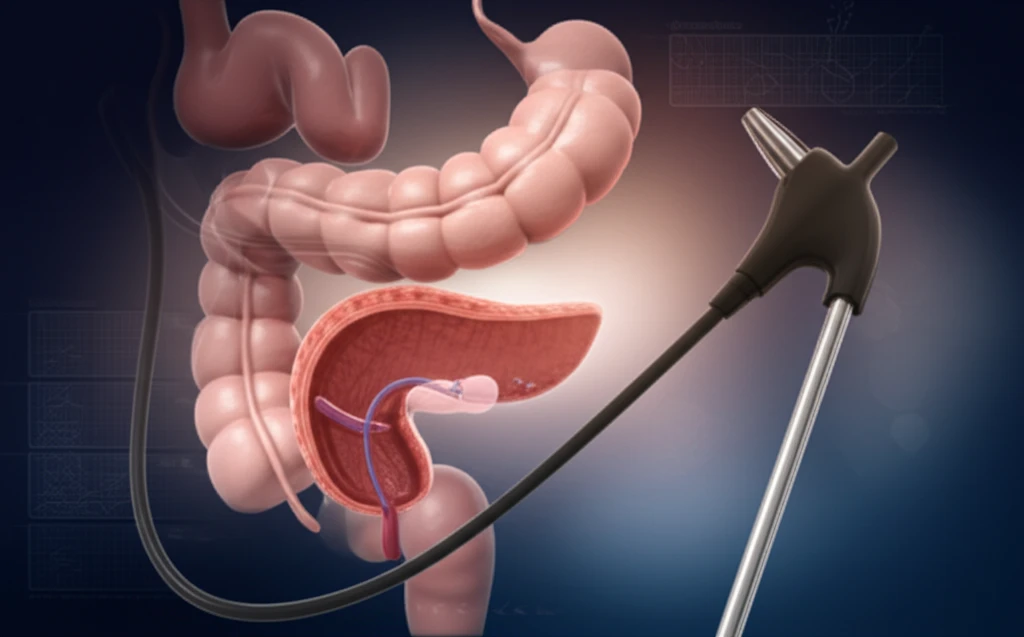
Digestive health is a cornerstone of overall well-being, and when issues arise, understanding the medical procedures designed to address them becomes paramount. Two such procedures, ERCP and cholecystectomy, are often intertwined in the treatment of biliary and gallbladder problems. ERCP, or Endoscopic Retrograde Cholangiopancreatography, is a procedure used to diagnose and treat issues in the bile ducts, gallbladder, and pancreas. Cholecystectomy, on the other hand, is the surgical removal of the gallbladder. When these two procedures are part of a patient's treatment plan, their timing can significantly impact recovery and long-term health.
Recent research highlights the importance of optimizing the sequence and timing of ERCP and cholecystectomy. This article aims to demystify the relationship between these two procedures, providing a clear and accessible guide for those seeking information. We'll explore the latest findings, the perspectives of medical experts, and the practical implications for patients and their families. Our goal is to empower you with knowledge so that you can make informed decisions and advocate for your health.
This is particularly relevant because the timing of these procedures can vary widely depending on the healthcare setting, the severity of the condition, and other factors. Understanding the rationale behind the recommended timelines and what factors influence them is crucial. This information can help you ask the right questions, understand the choices your healthcare providers are making, and actively participate in your treatment plan.
The ERCP-Cholecystectomy Connection: Why Timing Matters
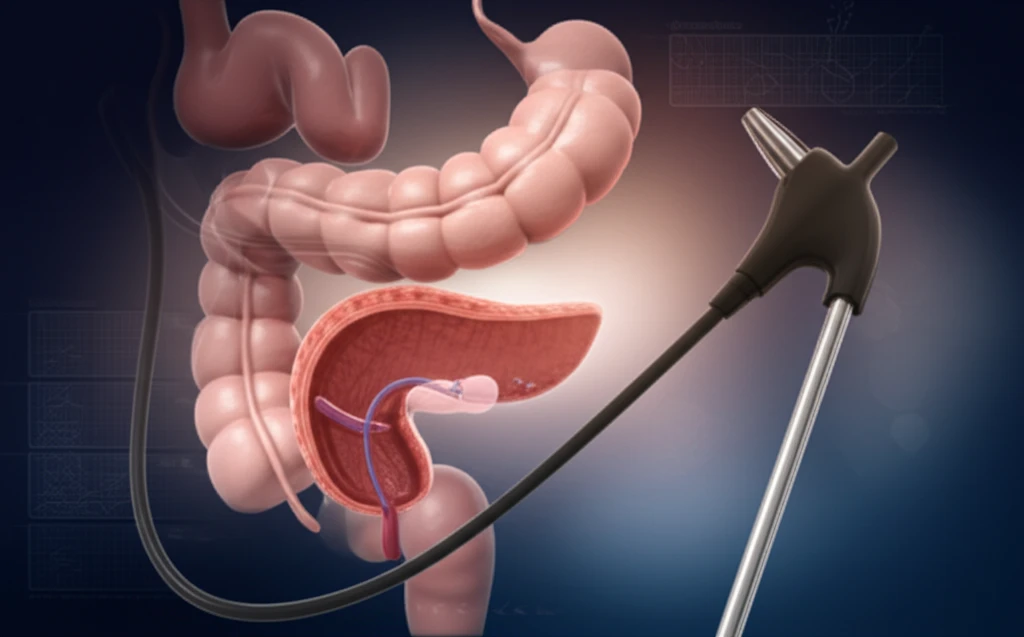
The interplay between ERCP and cholecystectomy often revolves around the diagnosis and treatment of gallstones and other biliary issues. ERCP is often used to clear blocked bile ducts or remove stones before a cholecystectomy. In many cases, ERCP is performed first to address any immediate blockages or infections, followed by cholecystectomy to remove the gallbladder, the source of the problem. However, the exact sequence and the interval between these procedures are critical.
- Reduced Hospital Stays: Coordinated scheduling often results in shorter hospital stays, improving patient comfort and reducing healthcare costs.
- Lower Complication Rates: Properly timed procedures can help decrease the risk of complications.
- Faster Recovery: Synchronized care can contribute to a quicker and smoother recovery process.
Empowering Your Digestive Health Journey
Understanding the nuances of ERCP and cholecystectomy timing is a significant step in taking control of your digestive health. By being informed, asking questions, and working closely with your healthcare team, you can actively participate in the process and contribute to a positive outcome. Remember, healthcare is a partnership, and your proactive involvement makes all the difference. This guide provides a solid foundation for informed decision-making, helping you navigate the complexities of biliary issues with confidence and knowledge.
