Decoding Dialysis: How Nutrition and Strength Impact Patient Outcomes
"A comprehensive look into recent studies reveals the critical role of nutrition, inflammation, and physical strength in managing chronic kidney disease and improving survival rates for dialysis patients."
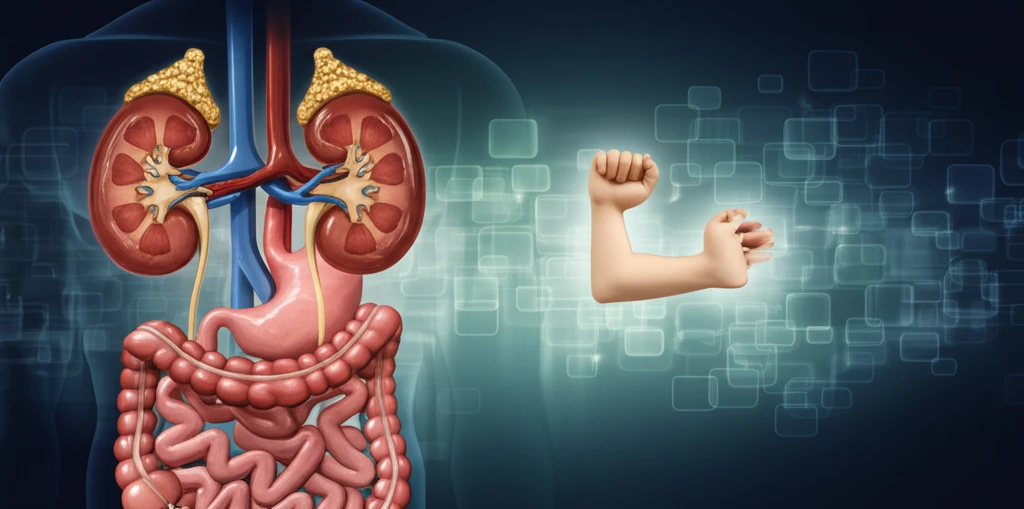
Chronic kidney disease (CKD) presents numerous challenges, impacting not only kidney function but also overall health. Patients undergoing dialysis, a life-sustaining treatment, often face additional complications related to nutrition, inflammation, and physical strength. Recent studies shed light on these critical factors, offering insights into how healthcare providers can better support and improve patient outcomes.
Malnutrition and inflammation are common in dialysis patients and can significantly affect their quality of life and survival rates. Understanding the interplay between these elements is crucial for developing effective treatment strategies. Moreover, simple assessments like handgrip strength are emerging as valuable tools for predicting patient survival and guiding personalized interventions.
This article delves into the findings of several key research papers, highlighting the importance of gastrointestinal microbiota, nutritional status, inflammation markers, and handgrip strength in managing CKD. By examining these factors, we can gain a clearer understanding of how to optimize patient care and enhance their overall well-being.
The Gut-Kidney Connection: Optimizing Gastrointestinal Microbiota in CKD
The gastrointestinal (GI) microbiota plays a significant role in the health of individuals with chronic kidney disease (CKD). Emerging research indicates that alterations in the GI microbiota can impact circulating metabolites, exacerbate symptoms, and affect the overall quality of life for CKD patients. A systematic review by Barnes, Chung, and Schafer Astroth aimed to evaluate the data on GI microbiota in CKD patients and the potential impact of prebiotic and/or probiotic interventions.
- Dysbiosis: CKD patients show a distinct dysbiosis (imbalance) in their gut microbiota compared to healthy individuals.
- Proteolytic Bacteria: An increase in proteolytic bacteria contributes to uremic toxin production.
- Prebiotics and Probiotics: Supplementation may help restore a more beneficial microbial profile.
Empowering Patients Through Comprehensive Care
The studies examined underscore the importance of a holistic approach to managing chronic kidney disease. By integrating regular nutritional assessments, monitoring inflammation, and incorporating simple functional tests like handgrip strength measurements, healthcare providers can gain valuable insights into patient health and tailor interventions to improve outcomes. Ultimately, empowering patients with knowledge and support can lead to better quality of life and increased survival rates.
