Decoding Diabetes: How a Unified View Can Transform Treatment
"Exploring the Pathophysiological Construct of Diabetes and its Complications for Better Management."
Diabetes mellitus, a widespread metabolic disorder, poses a significant global health challenge. Its complexity stems from a variety of factors, including genetics, lifestyle, and environmental influences, all of which contribute to its diverse clinical presentations and complications. Managing diabetes effectively requires a comprehensive understanding of these interconnected elements.
Traditional approaches to diabetes often treat individual symptoms or complications in isolation. However, emerging research emphasizes the need for a holistic perspective that acknowledges the interplay between various physiological systems. This "unified pathophysiological construct" offers a more integrated way to understand diabetes, potentially leading to more effective and personalized treatment strategies.
This article delves into the unified pathophysiological construct of diabetes, examining how it can revolutionize our understanding of the disease and its complications. By exploring the interconnectedness of different factors, we aim to provide insights that empower individuals, healthcare professionals, and researchers to tackle diabetes with greater precision and success.
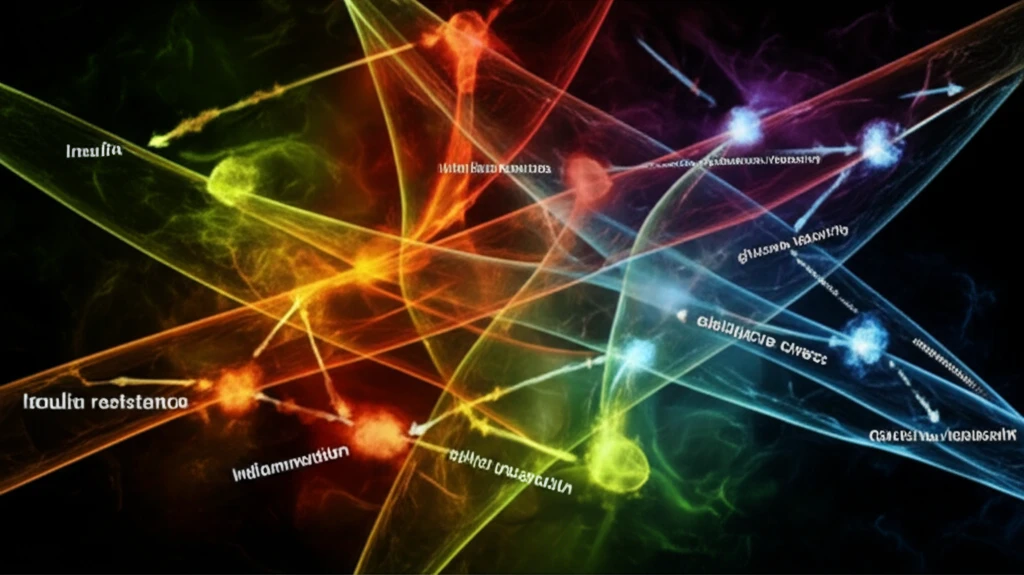
What is the Unified Pathophysiological Construct of Diabetes?
The unified pathophysiological construct is a framework that integrates various aspects of diabetes, including insulin resistance, insulin deficiency, glucose toxicity, inflammation, and oxidative stress, into a cohesive model. It acknowledges that these factors are not independent but rather interconnected and synergistic in their effects on the body.
- Glucose Toxicity: High blood sugar levels can damage cells and tissues throughout the body, contributing to complications such as neuropathy, nephropathy, and retinopathy.
- Inflammation: Chronic inflammation is a key player in diabetes, exacerbating insulin resistance and damaging blood vessels, which increases the risk of cardiovascular disease.
- Oxidative Stress: An imbalance between the production of free radicals and the body's ability to neutralize them can lead to cellular damage and contribute to the progression of diabetes complications.
Taking a Holistic Approach to Diabetes Care
The unified pathophysiological construct represents a paradigm shift in diabetes management, moving away from a fragmented approach to a more integrated and holistic one. By recognizing the interconnectedness of various factors, healthcare professionals can develop more effective and personalized treatment strategies.
For individuals with diabetes, understanding this construct can empower them to take proactive steps in managing their condition. Lifestyle modifications, such as adopting a healthy diet, engaging in regular physical activity, and managing stress, can have a significant impact on improving insulin sensitivity, reducing inflammation, and lowering blood glucose levels.
As research continues to unravel the complexities of diabetes, the unified pathophysiological construct will likely evolve and become even more refined. This ongoing quest for knowledge promises to bring new and innovative approaches to diabetes care, ultimately improving the lives of millions affected by this chronic condition.
