Decoding Cholesterol: The Surprising Link Between Inflammation and Heart Health
"New research illuminates how inflammation, influenced by factors like metabolic syndrome and diet, plays a critical role in cholesterol management and cardiovascular health."
For years, cholesterol has been public enemy number one in the battle against heart disease. We’ve diligently counted milligrams, scrutinized food labels, and even turned to medication to keep those numbers in check. But what if the picture is more complex than we thought? Emerging research suggests that inflammation, a process often overlooked, may be a key player in the cholesterol-heart health connection.
This isn't about dismissing the importance of cholesterol. High levels of LDL cholesterol (the “bad” kind) still pose a risk. However, understanding the why behind elevated cholesterol – the underlying mechanisms that contribute to it – is crucial for more effective prevention and treatment. Inflammation, it turns out, can significantly impact how our bodies process cholesterol.
This article will explore the fascinating link between inflammation and cholesterol, drawing on recent studies that shed light on this complex relationship. We'll delve into how conditions like metabolic syndrome and dietary choices can fuel inflammation, ultimately affecting your heart health. More importantly, we'll discuss practical strategies you can implement to manage inflammation and take control of your cardiovascular well-being. This isn't just about numbers; it's about understanding your body and making informed choices for a healthier heart.
The Inflammation-Cholesterol Connection: What the Science Says
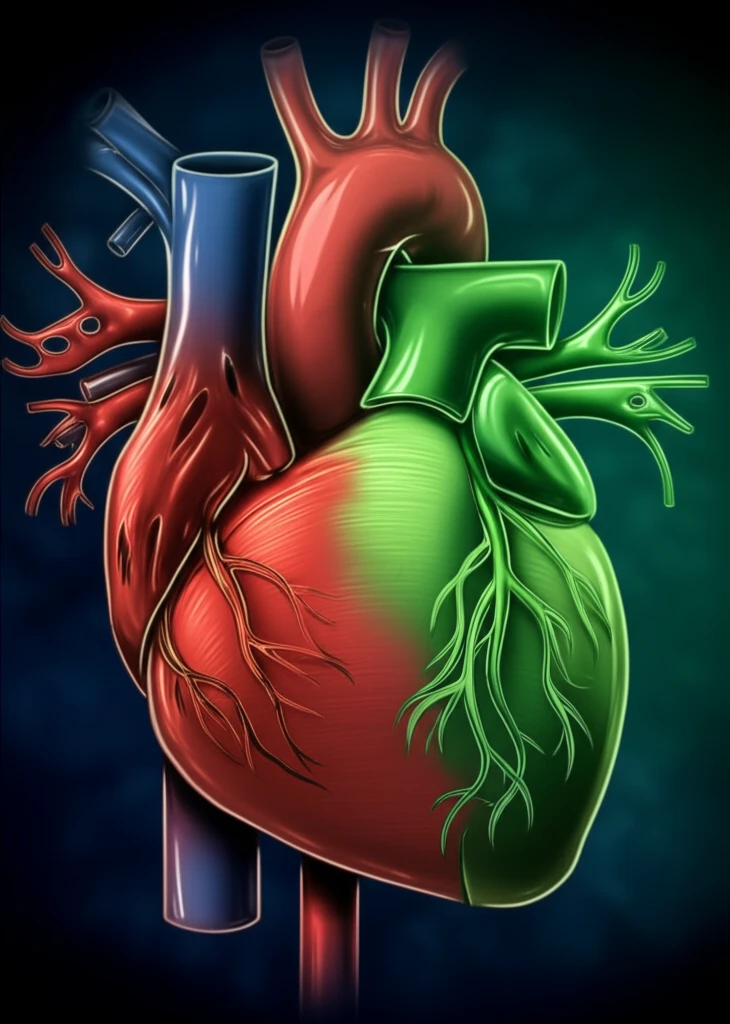
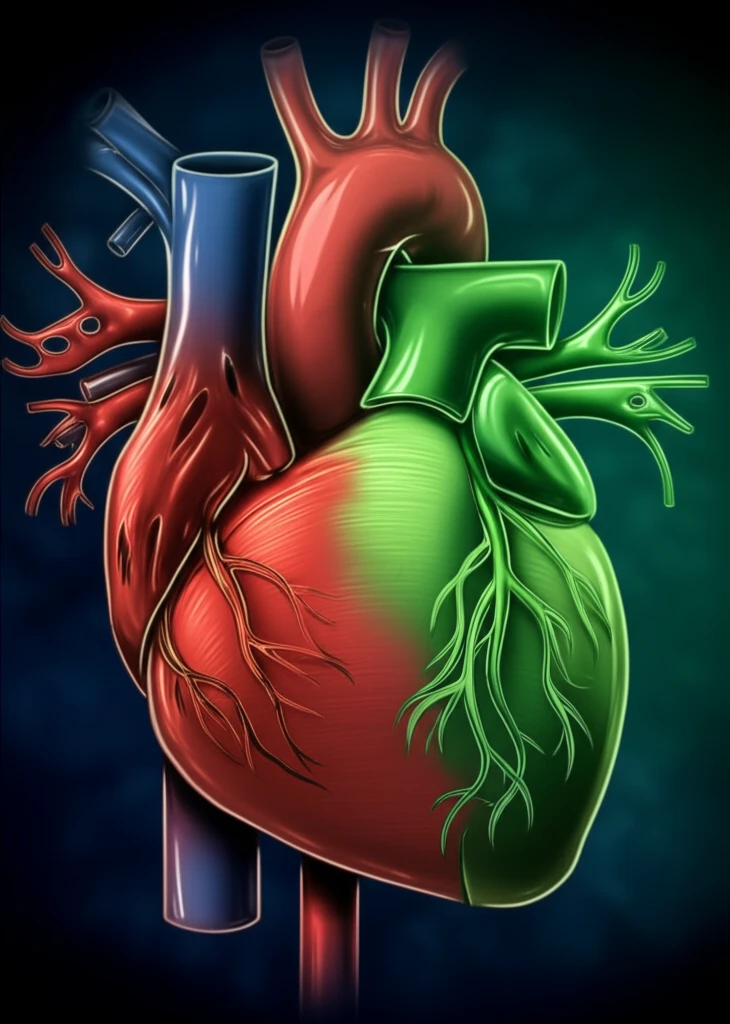
Several recent studies highlight the crucial role of inflammation in the development of atherosclerosis, the hardening and narrowing of the arteries that leads to heart disease and stroke. Atherosclerosis isn't simply about cholesterol buildup; it's an inflammatory process where immune cells become activated and contribute to plaque formation.
- Interleukin-17 (IL-17) and Metabolic Syndrome: A study investigating the link between Interleukin-17 (IL-17), an inflammatory cytokine, and metabolic syndrome (MS) found significantly higher IL-17 levels in MS patients. Importantly, these elevated IL-17 levels were correlated with increased carotid intima-media thickness (IMT), a marker of early atherosclerosis. This suggests that IL-17 contributes to preclinical vascular damage in individuals with metabolic syndrome.
- Uric Acid and Carotid Disease: Research examining the relationship between serum uric acid (SUA) and carotid artery disease in patients with atherosclerotic ischemic stroke revealed a significant correlation between SUA levels and IMT. Higher SUA levels were an independent predictor of increased IMT, even after adjusting for other cardiovascular risk factors. This indicates that SUA, potentially through its inflammatory effects, contributes to the progression of carotid disease.
- Postprandial Inflammation and Dietary Fat: A study comparing patients with primary hypercholesterolemia (PHC) and healthy controls investigated the postprandial (after-meal) inflammatory response to an oral fat load. PHC patients exhibited higher fasting levels of inflammatory markers. While the study observed a trend toward reduced inflammation in PHC patients after the oral fat load, more research is needed to fully understand the impact of dietary fat on inflammation in this population.
- T-Cells and Atherosclerotic Plaques: Another study focused on the role of T-cells in atherosclerotic plaques. The researchers found that oxidized low-density lipoprotein (OxLDL) and malondialdehyde conjugated with human serum albumin (MDA-HSA) promote T-cell activation and differentiation into pro-inflammatory subtypes. Inhibiting mitochondrial reactive oxygen species (ROS) reduced T-cell activation, suggesting that oxidative stress plays a key role in this process.
- Nordic Walking and Antioxidant Defense: A study on patients with intermittent claudication (leg pain due to poor circulation) demonstrated that a 12-week Nordic walking program improved blood antioxidant defense. Nordic Walking significantly increased superoxide dismutase (SOD) activity and uric acid concentration while decreasing lipid peroxides. The training also improved walking ability.
Taking Control: Practical Steps to Reduce Inflammation and Protect Your Heart
The good news is that inflammation isn't an insurmountable foe. By adopting a heart-healthy lifestyle, you can significantly reduce inflammation and improve your cholesterol profile. Here are some actionable steps you can take today: <b>Embrace an Anti-Inflammatory Diet:</b> Focus on whole, unprocessed foods like fruits, vegetables, whole grains, and fatty fish rich in omega-3 fatty acids. Limit your intake of processed foods, sugary drinks, and unhealthy fats, which can promote inflammation. <b>Manage Your Weight:</b> Obesity, especially abdominal obesity, is a major driver of inflammation. Losing even a small amount of weight can make a big difference. <b>Get Regular Exercise:</b> Physical activity is a powerful anti-inflammatory. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Consider activities like Nordic walking, which has been shown to boost antioxidant defenses. <b>Quit Smoking:</b> Smoking is a potent inflammatory trigger. Quitting smoking is one of the best things you can do for your heart health. <b>Manage Stress:</b> Chronic stress can contribute to inflammation. Practice stress-reducing techniques like yoga, meditation, or spending time in nature. <b>Consider Targeted Supplements:</b> In some cases, supplements like omega-3 fatty acids, curcumin, or probiotics may help reduce inflammation. Talk to your doctor before starting any new supplements. It's also important to work with your healthcare provider to manage any underlying conditions like metabolic syndrome or high uric acid levels. Regular checkups and appropriate medical management can help keep inflammation in check and protect your heart.
