Decoding Breast Biopsy Results: How to Ensure Accuracy and Peace of Mind
"Understanding imaging-pathology concordance for accurate breast health diagnosis and management after ultrasound-guided biopsy."
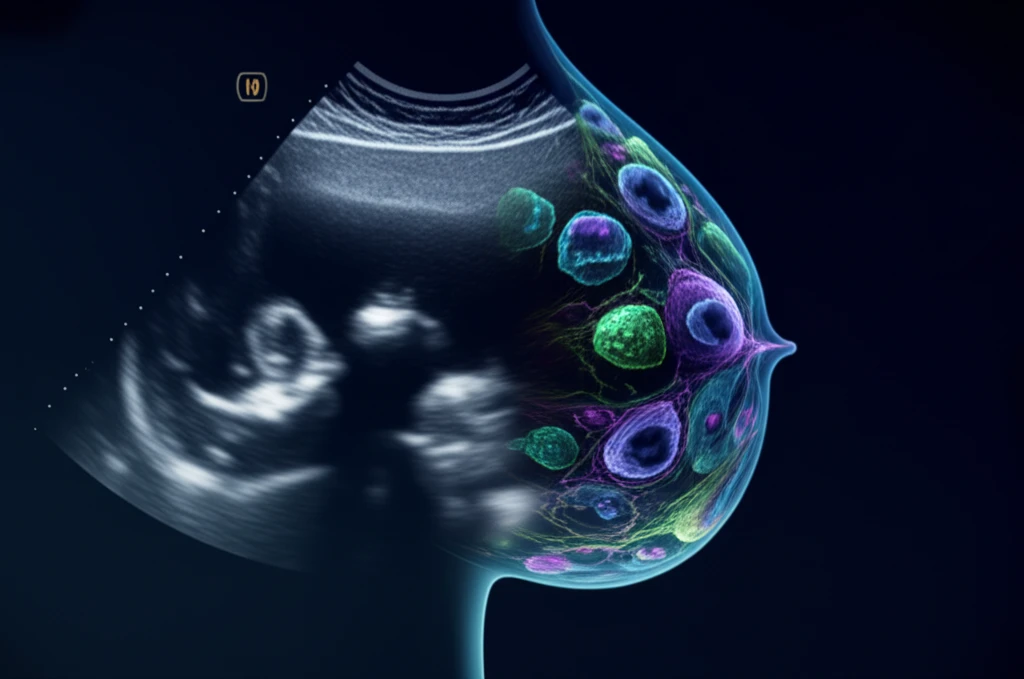
Ultrasound (US)-guided breast biopsy has become a cornerstone in diagnosing breast conditions due to its high diagnostic accuracy, approaching the reliability of open surgical biopsies. However, confirming adequate tissue retrieval after a US-guided biopsy remains a challenge, making false-negative results a possibility.
A critical step in validating biopsy results and guiding appropriate patient care is determining imaging-pathology concordance – essentially, ensuring that what the images show aligns with what the pathology report reveals. This process helps to minimize errors and ensures patients receive the correct diagnosis and treatment plan.
This article will explore the results of US-guided breast biopsies, discuss key considerations for establishing imaging-pathology concordance, review various categories of imaging-pathology correlations, and outline appropriate management strategies for each scenario. Understanding these elements can empower patients and healthcare providers to make informed decisions.
What is Imaging-Pathology Concordance and Why Does it Matter?
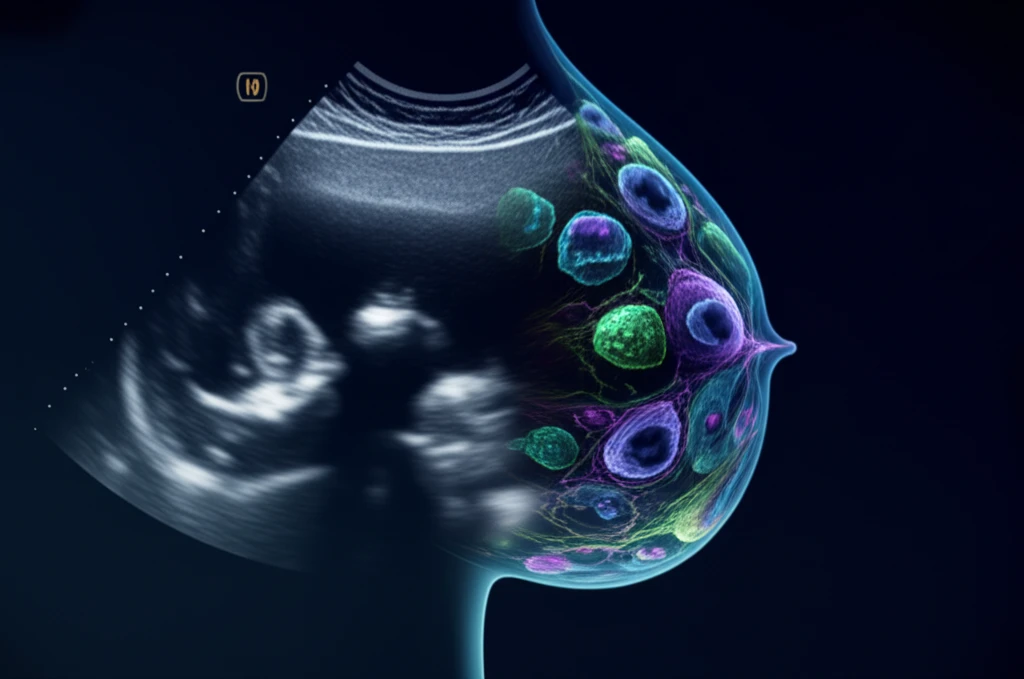
Imaging-pathology concordance refers to the agreement between the findings on breast imaging (such as ultrasound) and the results of the pathology analysis performed on the tissue sample obtained during a biopsy. When the imaging and pathology results align, it strengthens the confidence in the diagnosis.
- Inadequate Targeting: The biopsy needle may not have accurately targeted the suspicious area seen on the imaging.
- Sampling Error: The tissue sample obtained may not be representative of the entire lesion, especially if the lesion is heterogeneous.
- Technical Difficulties: Poor visualization of the lesion or needle during the procedure, dense breast tissue, or lesion mobility can hinder accurate targeting.
- Interpretative Errors: Discrepancies can arise from errors in interpreting either the imaging findings or the pathology results.
Ensuring Accuracy: A Collaborative Approach
Given the potential for discordance and its impact on patient care, a collaborative approach is crucial. This involves open communication between the radiologist performing the biopsy, the pathologist interpreting the tissue sample, the referring physician, and the patient.
When imaging-pathology discordance is suspected, the team should discuss the case, review the images and pathology slides, and consider whether additional tissue sampling is needed. This may involve a repeat biopsy using a different technique, such as vacuum-assisted breast biopsy (VABB), or surgical excision for a more comprehensive evaluation.
Ultimately, the goal is to ensure an accurate diagnosis and appropriate management plan, providing patients with the best possible care and peace of mind.
