Decoding Back Pain: How Neuroinflammation Could Be the Key to Relief
"New research sheds light on the role of neuroinflammation in chronic low back pain, offering potential new avenues for diagnosis and treatment."
Chronic low back pain is one of the most pervasive health problems worldwide, affecting a significant portion of the adult population. It's more than just an ache; it's a leading cause of disability, impacting daily life and productivity. Managing chronic back pain can feel like navigating a maze, with treatments often providing only temporary relief.
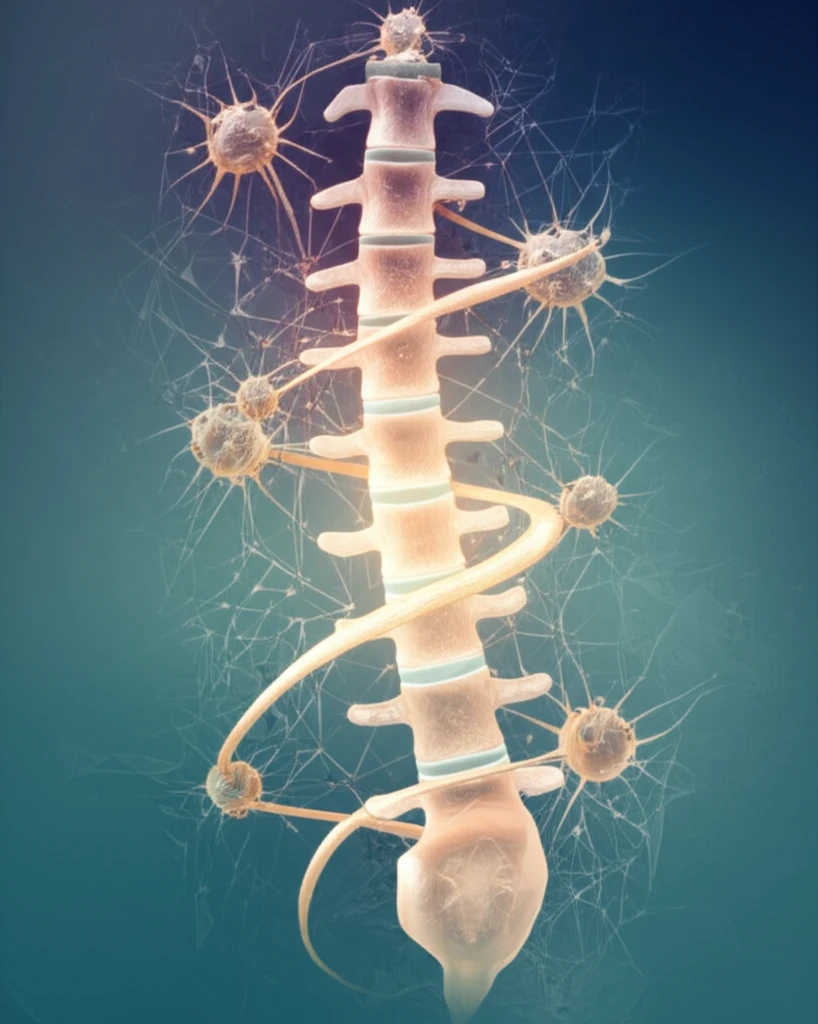
Imagine a scenario where the source of your chronic back pain isn't just structural, but also involves your nervous system's inflammatory response. Recent research suggests that neuroinflammation – inflammation within the nervous system – plays a critical role in many cases of chronic low back pain. Understanding this connection is key to developing more effective treatments.
This article delves into the exciting new findings about neuroinflammation and its connection to chronic low back pain. We'll explore the latest research, what it means for you, and the potential future of pain management. Get ready to discover how this knowledge could pave the way for a pain-free future.
The Neuroinflammation Connection: What the Research Reveals
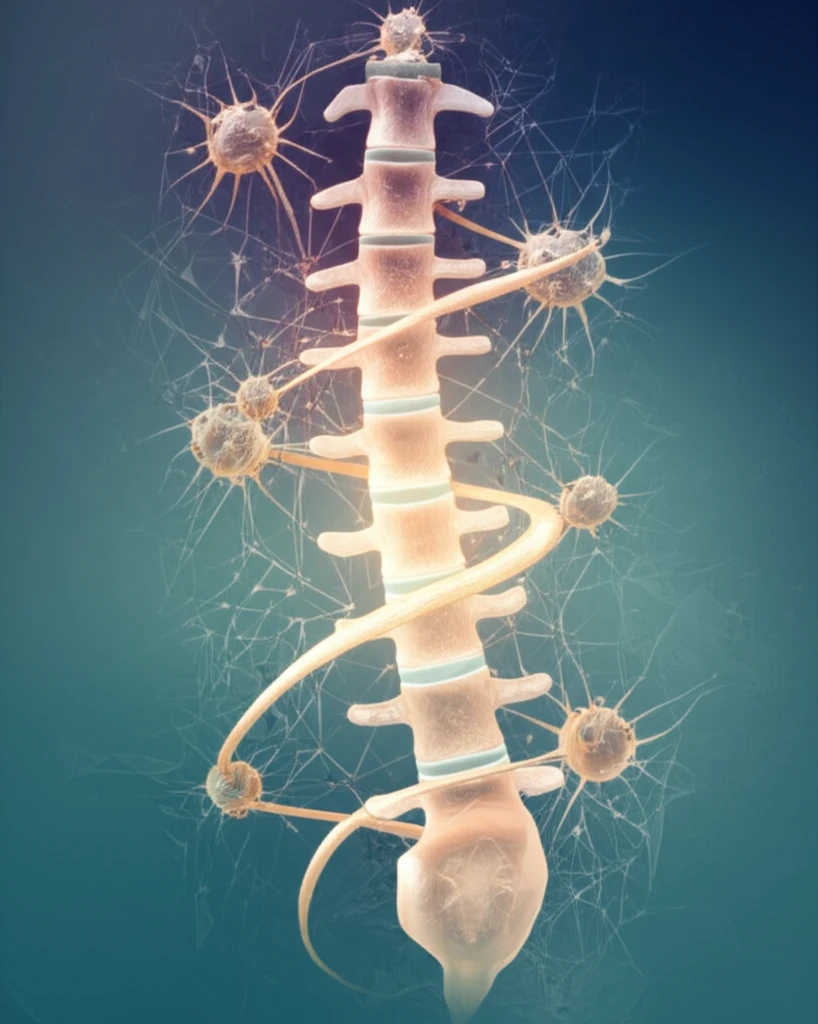
Traditionally, low back pain has been attributed to issues like disc degeneration, joint problems, or muscle strain. However, mounting evidence suggests that the nervous system's response to these issues can significantly amplify and prolong pain. Neuroinflammation occurs when the immune cells in the nervous system become activated, releasing inflammatory substances that sensitize pain pathways.
- IL-8 Levels: Significantly higher in patients with lumbar disc herniation (LDH).
- Cerebrospinal Fluid (CSF): Elevated IL-8 levels found in both male and female patients with LDH.
- Gender Differences: IL-8 levels correlated with pain scores in male patients only.
- Source of IL-8: Primarily produced by microglia and macrophages, key immune cells in the nervous system.
- Receptor Locations: Cognate receptors (CXCR1/2) are expressed on microglia, astrocytes, and pain projection neurons in the spinal cord.
The Future of Back Pain Relief: Targeting Neuroinflammation
Understanding the role of neuroinflammation in chronic low back pain opens up exciting new possibilities for treatment. Future therapies might focus on reducing inflammation within the nervous system, potentially providing more effective and long-lasting relief. This could involve novel drugs, targeted therapies, or lifestyle changes designed to modulate the immune response. While more research is needed, the discovery of the neuroinflammation connection marks a significant step forward in the fight against chronic back pain.
