CVC-Directed Thrombolysis: A Game-Changer in Massive Pulmonary Embolism?
"Learn how a central venous catheter (CVC) can deliver life-saving treatment directly to pulmonary embolisms, improving outcomes in critical cases."
Pulmonary embolism (PE) is a life-threatening condition where blood clots block arteries in the lungs, leading to severe cardiovascular issues. Emergency physicians frequently encounter PE, which can range from minor blockages to massive saddle emboli causing circulatory collapse. Traditionally, thrombolysis (dissolving the clot with medication) and surgical thrombectomy (removing the clot surgically) are reserved for severe cases of PE, particularly when patients experience persistent hypotension or shock.
Administering thrombolytic therapy in hemodynamically unstable patients with confirmed or suspected PE is a balancing act. The American College of Emergency Physicians (ACEP) recommends thrombolysis for confirmed PE cases where the benefits outweigh the risks of bleeding. They also suggest considering it for unstable patients when a PE diagnosis is highly suspected but cannot be immediately confirmed. The challenge lies in quickly and effectively delivering the medication to dissolve the clot and restore blood flow.
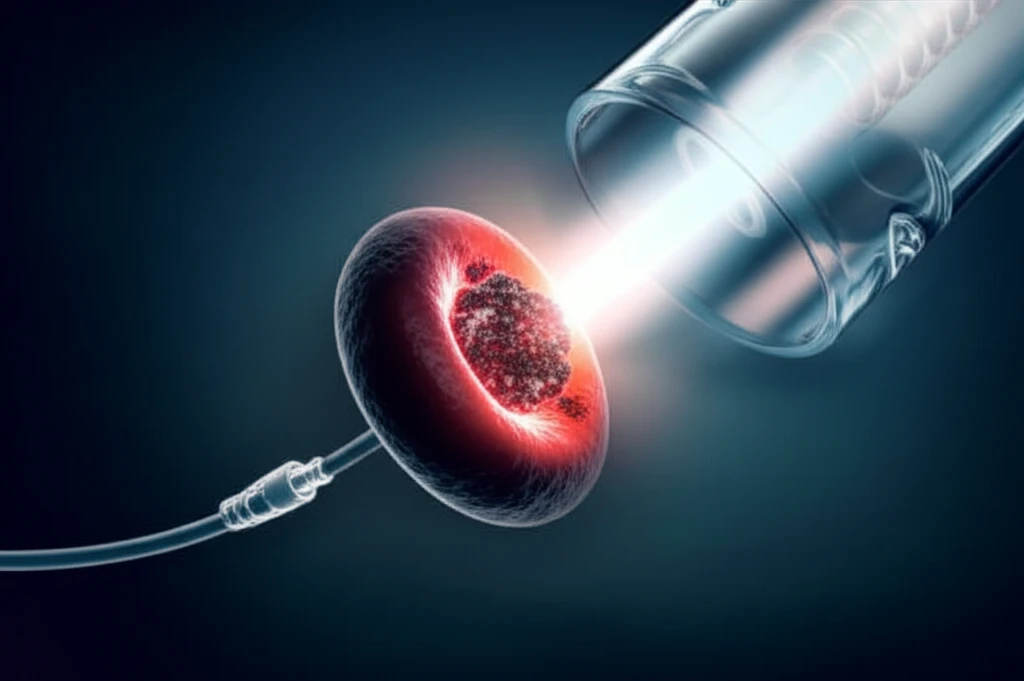
A recent case highlights a novel approach to this challenge: using a central venous catheter (CVC) to deliver tissue plasminogen activator (tPA), a potent thrombolytic drug, directly to the pulmonary embolism. This method may offer advantages over traditional peripheral infusions, particularly in critical cases where rapid intervention is crucial.
What is CVC-Directed Thrombolysis and Why Does It Matter?
CVC-directed thrombolysis involves inserting a central venous catheter (CVC) into a large vein, typically in the neck or groin, and threading it close to the location of the pulmonary embolism. Instead of administering the thrombolytic drug through a peripheral IV line, it is injected directly through the CVC. This targeted approach aims to:
- Minimize systemic exposure to the drug, possibly reducing the risk of bleeding complications.
- Achieve quicker restoration of blood flow and improve patient outcomes, especially in cases of cardiac arrest or severe hemodynamic instability.
The Future of PE Treatment: Is CVC-Directed Thrombolysis the Answer?
The successful outcome in this case suggests that CVC-directed thrombolysis may be a valuable tool in the emergency physician's arsenal for treating massive PE, particularly in patients experiencing cardiac arrest or severe instability. While this approach shows promise, it's important to acknowledge that more research is needed. The authors of the original study themselves call for further investigation to analyze the effectiveness of CVC-directed tPA and its impact on morbidity and mortality. Randomized controlled trials comparing central versus peripheral thrombolysis are essential to determine the optimal route and dosage of thrombolytic drugs in these critical situations. For now, CVC-directed thrombolysis remains a promising but investigational technique that warrants consideration in select cases of massive PE.
