Cracking the Code: Understanding the Link Between Kidney Health, Mineral Imbalances, and Your Well-being
"Explore the complexities of Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) and how it impacts your health, from cardiovascular risks to the importance of personalized care."
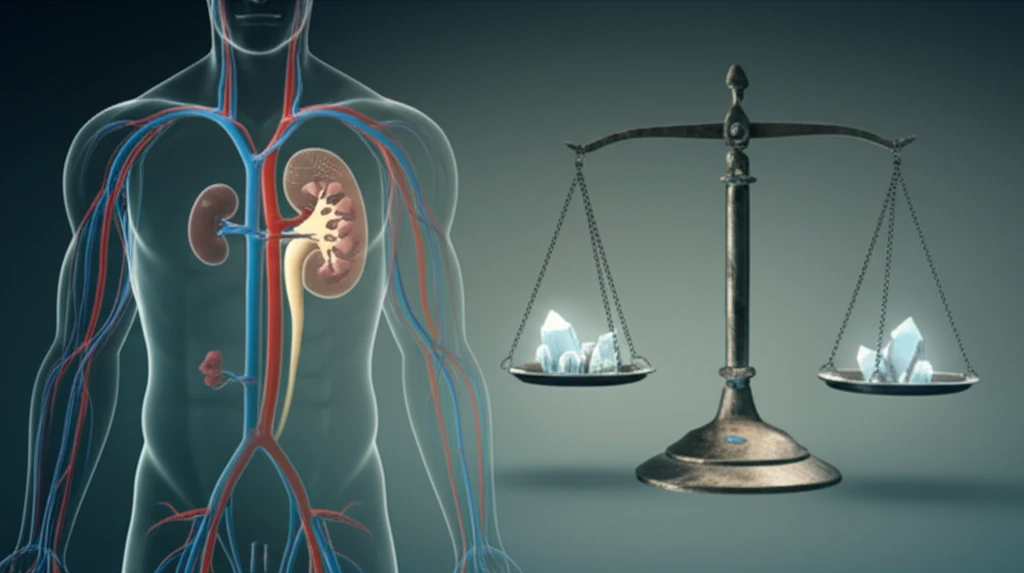
Kidney health is a cornerstone of overall well-being, yet it's often overlooked until problems arise. Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) represents a significant challenge, affecting millions worldwide. This condition highlights the intricate relationship between our kidneys, bone health, and the delicate balance of minerals in our blood. Understanding CKD-MBD isn't just for medical professionals; it's vital knowledge for anyone interested in proactive health management.
This article delves into the heart of CKD-MBD, exploring its impact on cardiovascular health, the global guidelines designed to manage it, and the gaps that exist between these guidelines and real-world practices. We'll examine how mineral imbalances, particularly those involving calcium, phosphorus, and parathyroid hormone (PTH), can affect your body. You'll also learn about the importance of personalized care and how to advocate for your health.
Whether you're seeking to understand a recent diagnosis, support a loved one, or simply expand your health knowledge, this article aims to demystify CKD-MBD. We'll provide accessible explanations, explore the latest research, and empower you with the information needed to make informed decisions about your health. Let's embark on a journey toward better kidney health together.
Decoding CKD-MBD: What You Need to Know
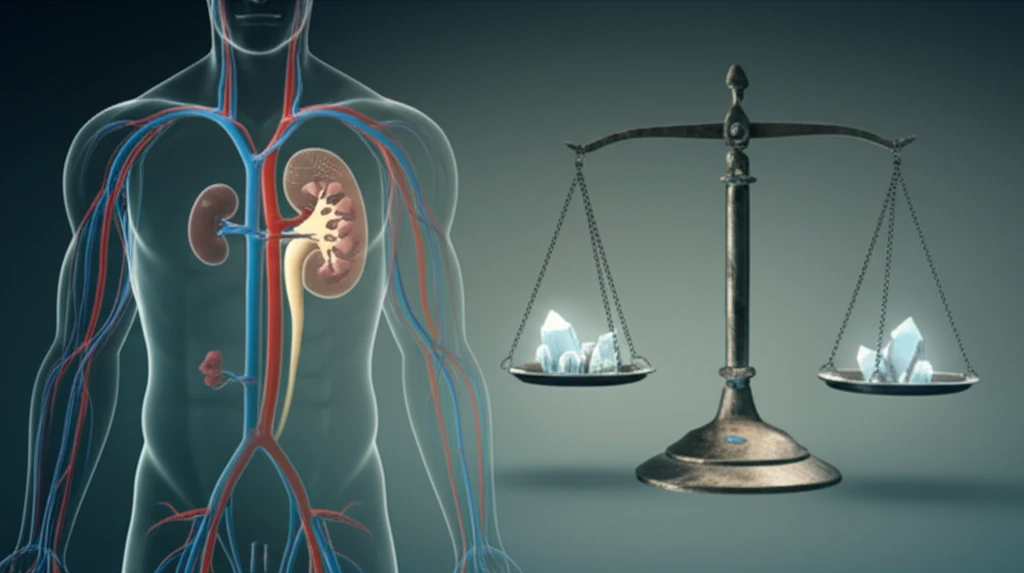
CKD-MBD is more than just a mouthful of medical jargon; it signifies a systemic disorder that affects multiple aspects of your health. The term itself evolved from 'renal osteodystrophy,' emphasizing the broader implications of the condition beyond bone health. The key lies in the interplay of your kidneys, bones, and crucial minerals like calcium, phosphorus, and PTH.
- Elevated Phosphorus: High phosphorus levels can lead to vascular calcification, hardening of the arteries, and increased risk of heart disease.
- Calcium Imbalance: Both high and low calcium levels can cause problems, affecting bone health and contributing to cardiovascular issues.
- Parathyroid Hormone (PTH): Elevated PTH is a response to mineral imbalances, but chronically high levels can further exacerbate bone and cardiovascular problems.
- Impact on Bones: CKD-MBD can weaken bones, increasing the risk of fractures and other skeletal issues.
Take Control: Your Path to Kidney Health
CKD-MBD may seem complex, but with knowledge comes empowerment. By understanding the interplay of minerals, the importance of personalized care, and the role of global guidelines, you can take an active role in your kidney health. Regular check-ups, open communication with your healthcare provider, and a proactive approach to managing your mineral levels are essential steps. This journey is not one you have to take alone. Seek support, ask questions, and stay informed. Your well-being is worth it.
