CO2 Embolism During Transanal TME: What Surgeons Need to Know
"A Deep Dive into Causes, Prevention, and Management Strategies for a Rare but Serious Complication."
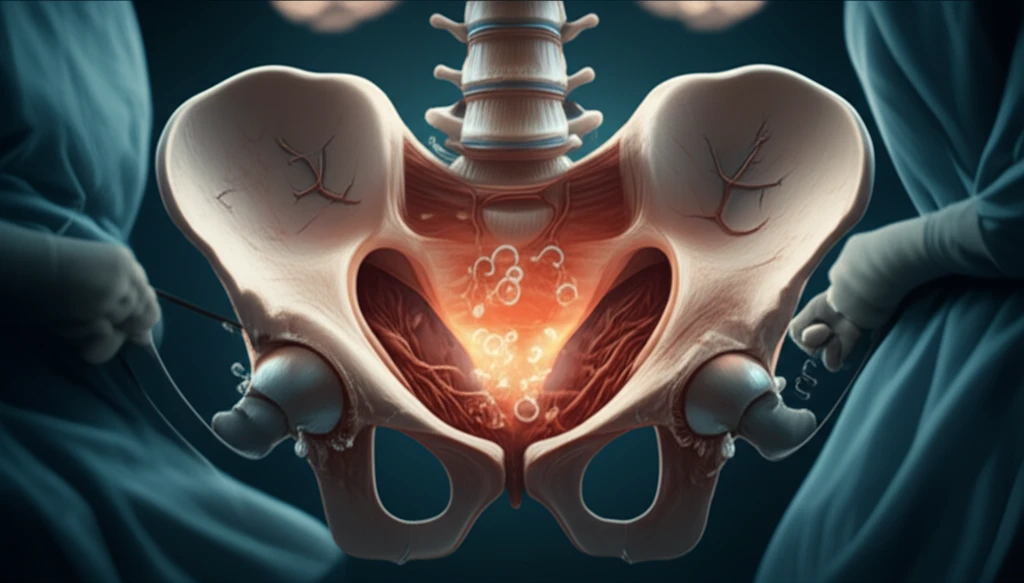
Transanal Total Mesorectal Excision (taTME) has revolutionized colorectal surgery, offering new hope for patients needing complex procedures. However, with any innovative technique comes a learning curve and the potential for unexpected complications. One such concern is carbon dioxide (CO2) embolism, a rare but serious event that can occur during the transanal phase of taTME.
While CO2 embolism is a known risk in laparoscopic surgery, it's considered negligible. Its occurrence during taTME, therefore, raises important questions about the unique factors at play. Recent studies have highlighted a few cases, prompting a closer look at the underlying causes and how to prevent them.
This article delves into the complexities of CO2 embolism during taTME, exploring the potential reasons behind its occurrence and offering practical strategies for surgeons to minimize this risk. Understanding these nuances is crucial for maximizing the benefits of taTME while ensuring the highest standards of patient safety.
Unmasking the Culprits: Why CO2 Embolism Occurs During taTME
The exact cause of CO2 embolism during taTME is likely multifactorial, involving a combination of factors that create a perfect storm. Let's break down the key elements that can contribute to this complication:
- Pneumo-pelvis Pressure: The pressure within the pneumo-pelvis can prevent small veins from collapsing completely when cut.
- AirSEAL® and Suction: The use of AirSEAL® for insufflation, combined with liberal suction, can create rapid changes in flow rates, promoting turbulent CO2 flow and increasing the likelihood of embolism.
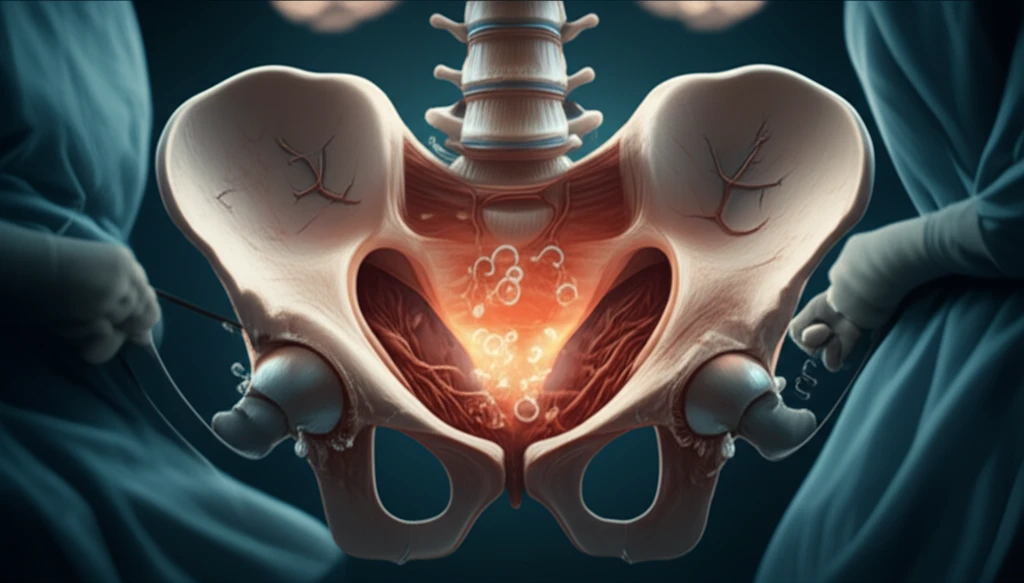
Practical Steps to Minimize CO2 Embolism Risk
While CO2 embolism is a rare complication, taking proactive steps is essential to protect patients during taTME procedures. By understanding the underlying causes, surgeons can implement strategies to minimize risk:
Applying gentle pressure with a gauze square during dissection, especially in the anterior region, can effectively aid haemostasis and reduce the need for aggressive suction. This approach minimizes turbulent CO2 flow and reduces the risk of venous entry.
By incorporating these strategies into their practice, surgeons can confidently offer the benefits of taTME while minimizing the risk of CO2 embolism. Continuous learning and adaptation are crucial for maximizing patient safety in this evolving surgical landscape.
