Checkpoint Inhibitors: The Future of Cancer Immunotherapy
"Discover how researchers are improving checkpoint inhibitors to maximize efficacy, minimize toxicity, and broaden their application in cancer treatment."
Cancer immunotherapy has emerged as a revolutionary approach in the fight against cancer, earning the title of 'Breakthrough of the Year' by Science in 2013. This groundbreaking field was further recognized with the Nobel Prize in Physiology or Medicine in 2018, awarded to James Allison and Tasuku Honjo for their pioneering work in establishing immune checkpoint pathways.
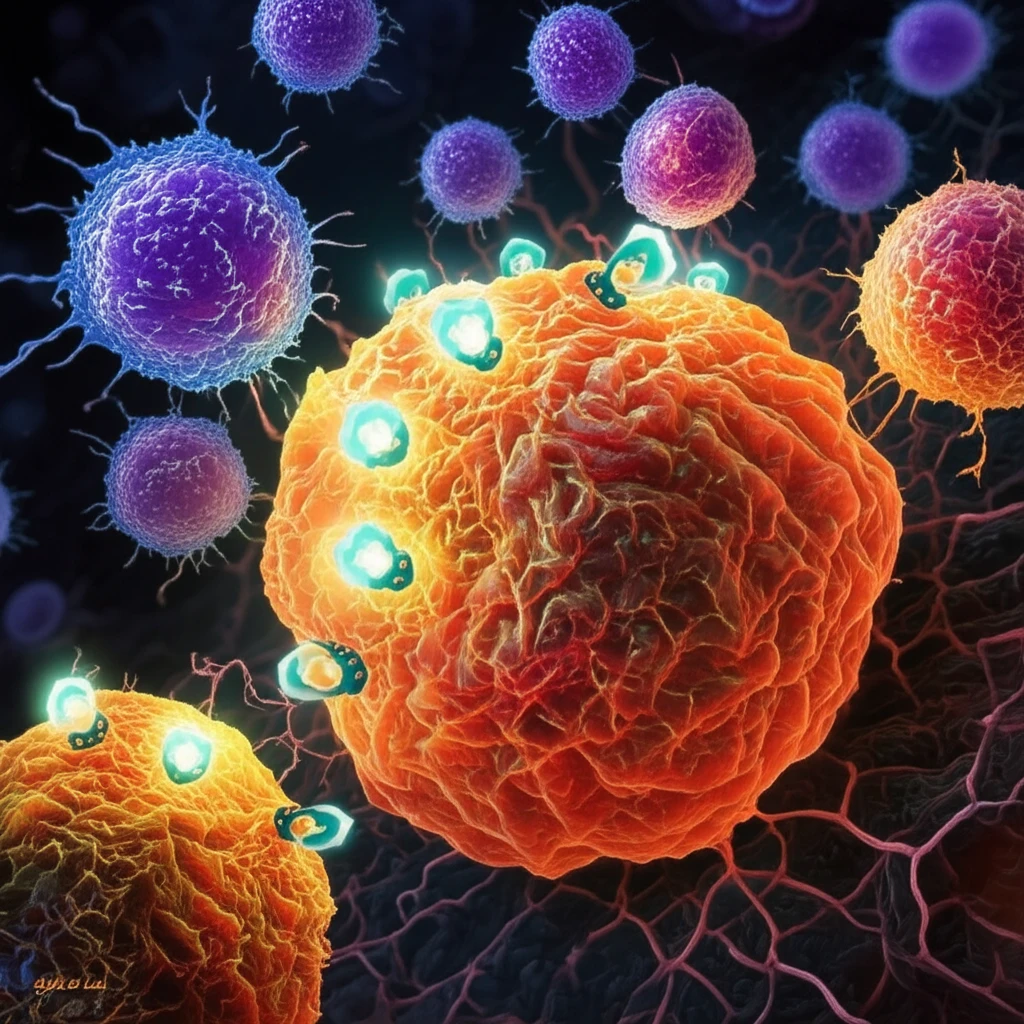
Allison and Honjo's research shed light on how immune checkpoint pathways act as 'brakes' on CD8+ T cells, which are crucial for destroying cancerous cells. By understanding and targeting these pathways, scientists have developed innovative strategies to unleash the full potential of the immune system in fighting cancer.
This article delves into the latest advancements in cancer immunotherapy, focusing on checkpoint inhibitors and their potential to revolutionize cancer treatment. We will explore how researchers are working to enhance their efficacy, reduce side effects, and expand the range of cancers they can treat.
Checkpoint Inhibitors: A New Era in Cancer Treatment
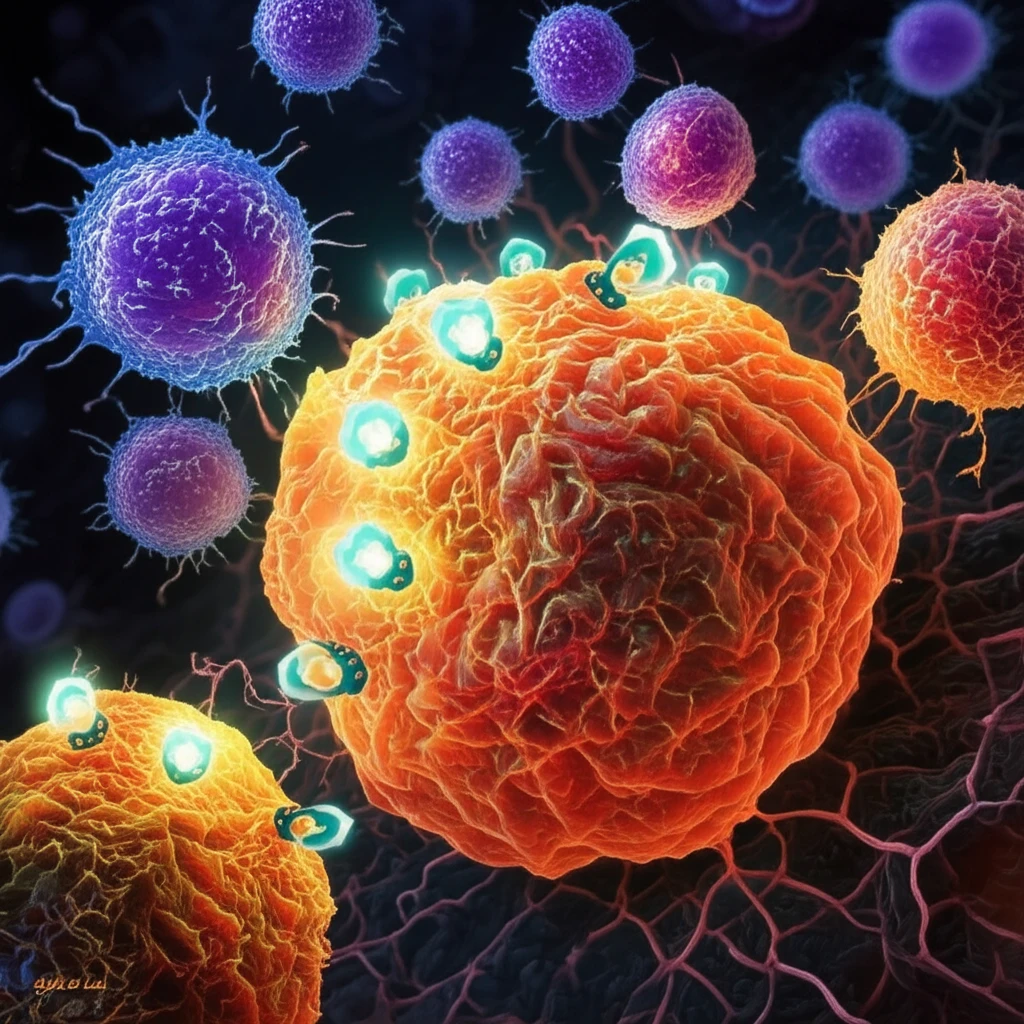
Checkpoint inhibitors have emerged as a promising class of cancer immunotherapies, demonstrating remarkable success in treating certain types of cancer. These inhibitors work by blocking specific proteins, known as immune checkpoints, that prevent T cells from attacking cancer cells. By blocking these checkpoints, the inhibitors unleash the T cells to recognize and destroy cancer cells.
- Pembrolizumab and nivolumab: These anti-PD-1 monoclonal antibodies bind to the PD-1 protein on T cells, preventing it from binding to PD-L1 on cancer cells.
- Atezolizumab: This checkpoint inhibitor targets PD-L1 on cancer cells, achieving the same effect as anti-PD-1 antibodies.
- Ipilimumab: This antibody targets CTLA-4, another immune checkpoint protein, and works in conjunction with anti-PD-1/PD-L1 agents.
The Future of Cancer Immunotherapy: Earlier, Safer, and More Effective
Researchers are exploring the use of checkpoint inhibitors in earlier stages of cancer, with the hope that these tumors may be more susceptible to immune attack. Additionally, efforts are underway to minimize the adverse inflammatory effects of immunotherapy, known as immune-related adverse events (irAEs).
One of the most promising areas of research is the development of personalized immunotherapy approaches. By identifying biomarkers that predict response to checkpoint inhibitors, clinicians can tailor treatment strategies to individual patients, maximizing the chances of success.
Despite the challenges, the future of cancer immunotherapy is bright. With ongoing research and innovation, checkpoint inhibitors and other immunotherapeutic approaches hold immense potential to transform cancer treatment and improve the lives of countless patients.
