CAR-T Cell Therapy: A Revolutionary Approach to Fighting Cancer
"Understanding Personalized Immunotherapy and Its Impact on Cancer Treatment"
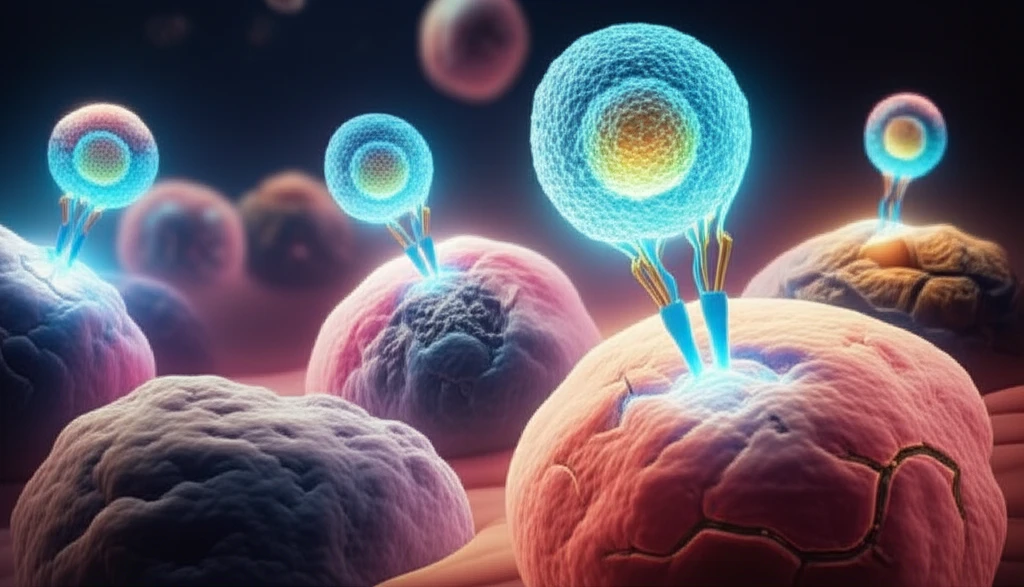
In the relentless battle against cancer, medical science continually seeks innovative treatments. Among the most promising advancements is CAR-T cell therapy, a form of immunotherapy that has revolutionized cancer treatment. This personalized approach utilizes the patient's own immune cells to target and destroy cancer cells, offering hope where traditional methods have faltered.
This article delves into the world of CAR-T cell therapy, exploring its mechanisms, clinical efficacy, potential side effects, and the future implications for cancer treatment. We'll break down the science behind this revolutionary treatment, making it accessible and understandable for everyone.
As we explore the intricacies of CAR-T cell therapy, we aim to empower you with knowledge. We'll discuss the latest developments, clinical trial results, and what this innovative therapy means for patients and their families.
How CAR-T Cell Therapy Works: A Step-by-Step Guide
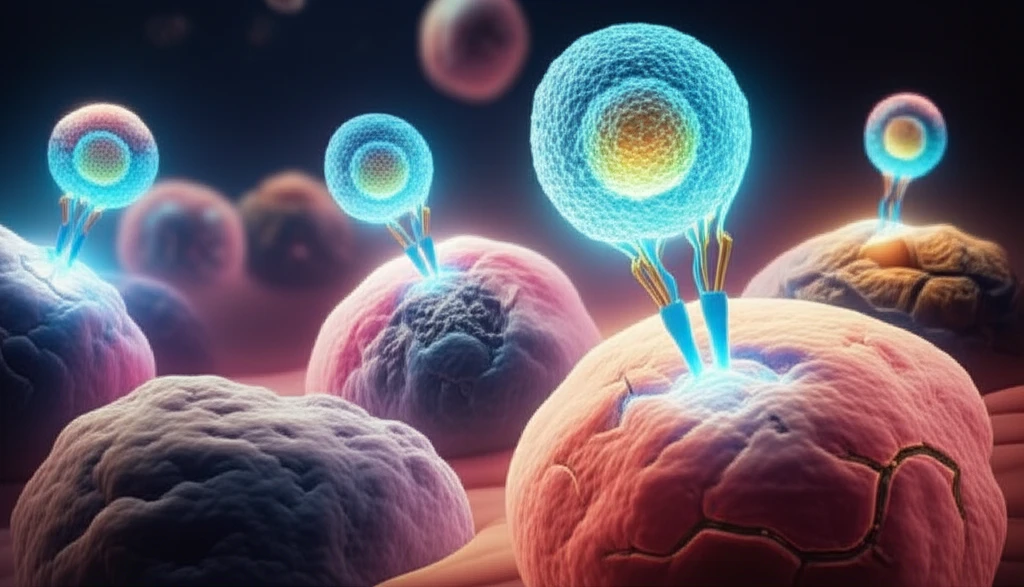
CAR-T cell therapy is a highly personalized treatment that involves several key steps. The process begins with collecting T cells from the patient's blood. These T cells are a type of white blood cell that plays a crucial role in the immune system.
- Collection: T cells are extracted from the patient's blood.
- Modification: The T cells are genetically engineered to express CARs.
- Expansion: The modified T cells are multiplied in the lab.
- Infusion: The CAR-T cells are infused back into the patient.
- Action: CAR-T cells bind to cancer cells and kill them.
The Future of CAR-T Cell Therapy
CAR-T cell therapy represents a significant leap forward in cancer treatment. Its potential to harness the body's own immune system to fight cancer is truly remarkable. While there are challenges, including the high cost and potential side effects, ongoing research and development are constantly improving the efficacy and safety of this innovative therapy. As we move forward, CAR-T cell therapy promises to be a key player in the future of cancer treatment, offering renewed hope for patients worldwide.
