CAR-T Cell Therapy: A Personalized Cancer Immunotherapy Game Changer?
"Explore how CAR-T cell therapy is revolutionizing cancer treatment with personalized immunotherapy, offering new hope for patients with leukemia and lymphoma."
In the realm of cancer treatment, personalized medicine is rapidly transforming the landscape, offering targeted therapies that are tailored to an individual's unique genetic makeup and disease characteristics. Among these innovative approaches, CAR-T cell therapy stands out as a groundbreaking form of immunotherapy that harnesses the power of a patient's own immune system to fight cancer.
Tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta), two CAR-T cell therapies, have already been licensed for the treatment of specific patient populations with leukemia or lymphoma, marking a significant milestone in the field of personalized cancer treatment. These therapies represent the forefront of a new wave of innovative approaches that are revolutionizing how we combat cancer.
This article delves into the intricate details of CAR-T cell therapy, exploring its innovative mechanism of action, clinical trial results, potential adverse effects, and its anticipated future role in cancer treatment. Discover how this personalized immunotherapy approach is offering new hope to patients with previously limited treatment options.
How Does CAR-T Cell Therapy Work?
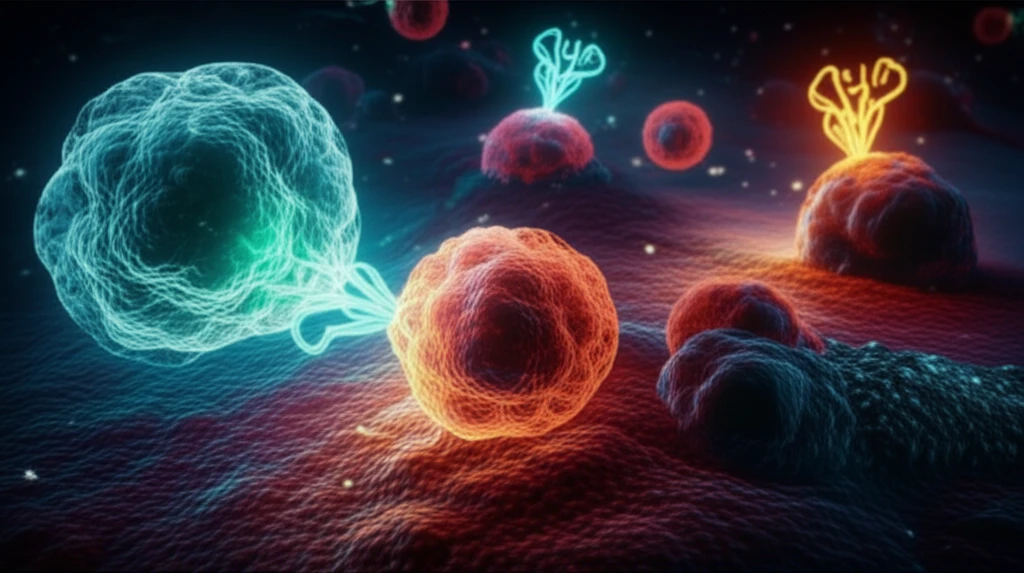
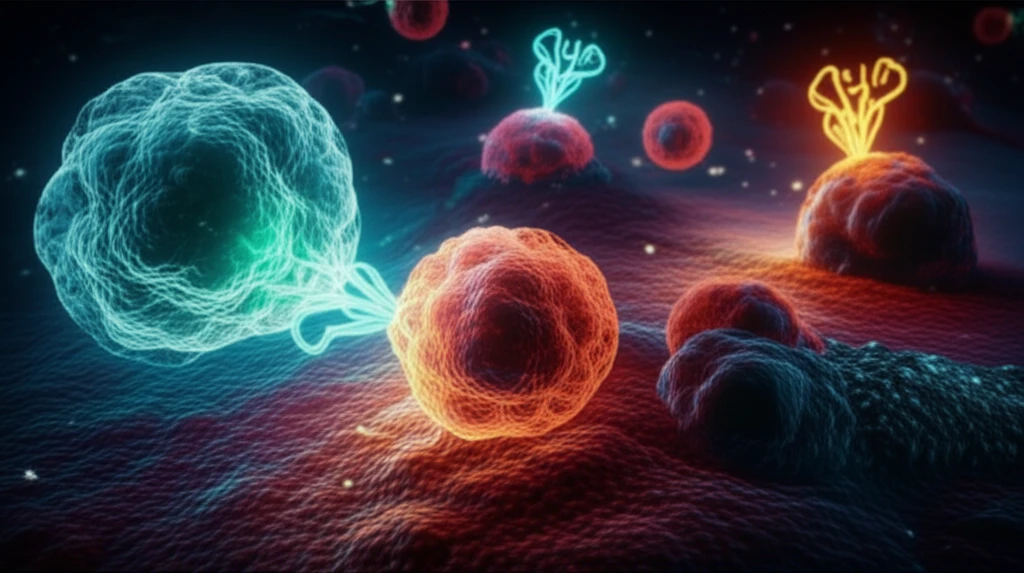
CAR-T cell therapy is a highly personalized treatment approach that involves modifying a patient's own T cells, a type of immune cell, to target and destroy cancer cells. This process begins with harvesting T cells from the patient's blood, followed by genetic modification in the laboratory to express a chimeric antigen receptor (CAR) on their surface.
- Harvesting T Cells: T cells are collected from the patient's blood through a process called apheresis.
- Genetic Modification: In the laboratory, a viral vector is used to introduce the gene encoding the CAR into the T cells. This allows the T cells to express the CAR on their surface.
- CAR-T Cell Expansion: The modified T cells, now called CAR-T cells, are expanded in the laboratory to generate a large number of cells.
- Infusion into Patient: The expanded CAR-T cells are infused back into the patient's bloodstream.
- Cancer Cell Recognition: The CAR-T cells circulate throughout the body, recognizing and binding to the CD19 antigen on cancer cells.
- Immune Response Activation: Upon binding to the cancer cells, the CAR-T cells become activated, triggering an immune response that leads to the destruction of the cancer cells.
The Future of CAR-T Cell Therapy
CAR-T cell therapy is a rapidly evolving field with immense potential to transform cancer treatment. While it has shown remarkable success in treating certain types of leukemia and lymphoma, ongoing research is focused on expanding its application to other cancers, including solid tumors. Overcoming the challenges associated with targeting solid tumors, such as limited CAR-T cell infiltration and immunosuppressive microenvironments, is a key area of investigation.
