CAR-T Cell Therapy: A New Dawn for Personalized Cancer Immunotherapy
"Explore how CAR-T cell therapy is revolutionizing cancer treatment, offering new hope for patients with leukemia and lymphoma by harnessing the power of their own immune systems."
The field of cancer treatment is constantly evolving, and one of the most promising recent advances is CAR-T cell therapy. This innovative approach harnesses the power of the patient's own immune system to fight cancer, offering new hope for individuals with certain types of leukemia and lymphoma. In this comprehensive guide, we'll delve into the intricacies of CAR-T cell therapy, exploring its mechanisms, clinical trial results, potential benefits, and challenges.
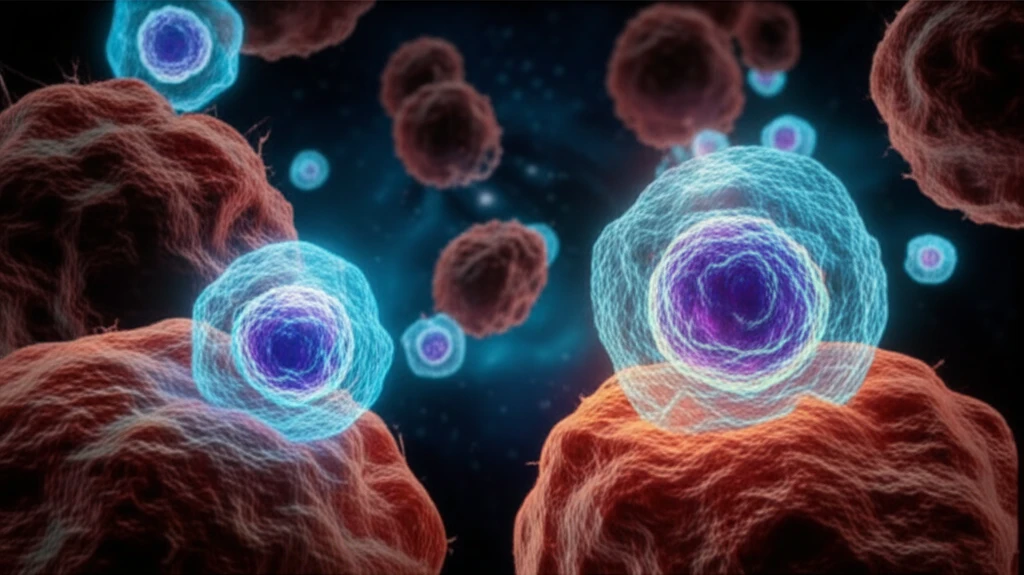
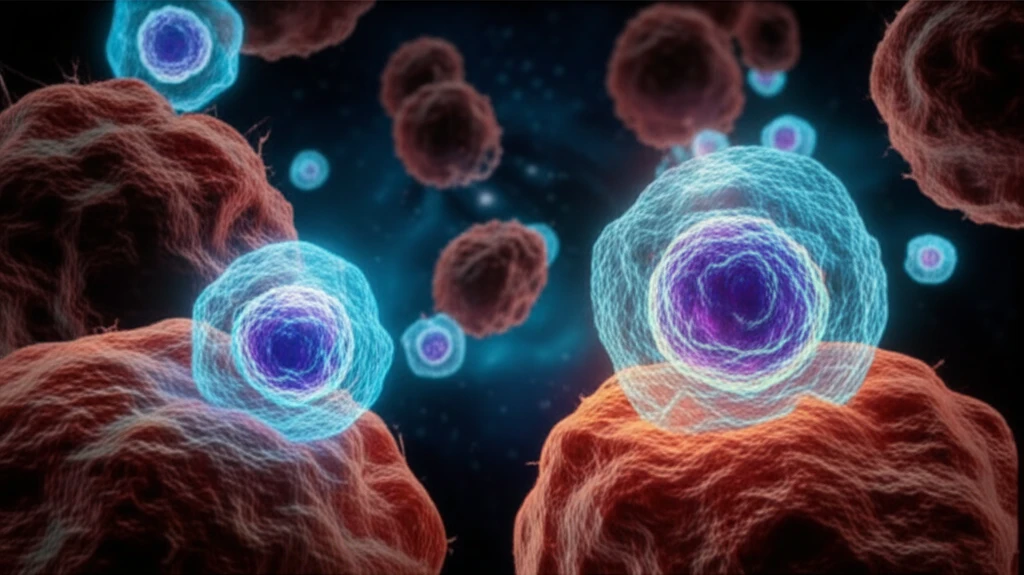
CAR-T cell therapy stands for Chimeric Antigen Receptor T-cell therapy. It involves modifying a patient's T cells, a type of immune cell, to express receptors that can recognize and bind to specific antigens (proteins) on cancer cells. These modified T cells, now equipped to target and destroy cancer cells, are then infused back into the patient.
Two CAR-T cell therapies, tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta), have already been licensed for the treatment of specific patients with leukemia and lymphoma. These therapies represent the forefront of personalized cancer treatments, offering a new wave of hope for those who have not responded to traditional therapies.
How Does CAR-T Cell Therapy Work?
CAR-T cell therapy is a complex process that involves several key steps:
- T Cell Collection: T cells are collected from the patient's blood through a process called apheresis.
- Genetic Modification: In the laboratory, the collected T cells are genetically modified using a viral vector. This vector introduces a gene that codes for a chimeric antigen receptor (CAR). The CAR is designed to recognize a specific antigen found on cancer cells, such as CD19, a protein commonly expressed on B-cell lymphomas and leukemias.
- Expansion: The modified T cells, now expressing the CAR, are expanded in the laboratory to create a large number of CAR-T cells.
- Infusion: The expanded CAR-T cells are infused back into the patient's bloodstream.
- Cancer Cell Targeting: Once infused, the CAR-T cells circulate throughout the body and seek out cancer cells expressing the target antigen.
- Activation and Destruction: When a CAR-T cell encounters a cancer cell with the target antigen, it binds to it, activating the CAR-T cell. This activation triggers the CAR-T cell to release cytotoxic molecules that kill the cancer cell.
The Future of CAR-T Cell Therapy
CAR-T cell therapy is a rapidly evolving field with immense potential to transform cancer treatment. Ongoing research is focused on expanding its application to other types of cancer, improving its safety and efficacy, and developing strategies to overcome resistance. As research progresses and technology advances, CAR-T cell therapy is poised to become an increasingly important tool in the fight against cancer, offering new hope and improved outcomes for patients worldwide.
