Can a Simple Blood Test Predict Outcomes in Nasopharyngeal Cancer?
"New research highlights the Systemic Inflammation Response Index (SIRI) as a valuable tool for personalized treatment in nasopharyngeal carcinoma."
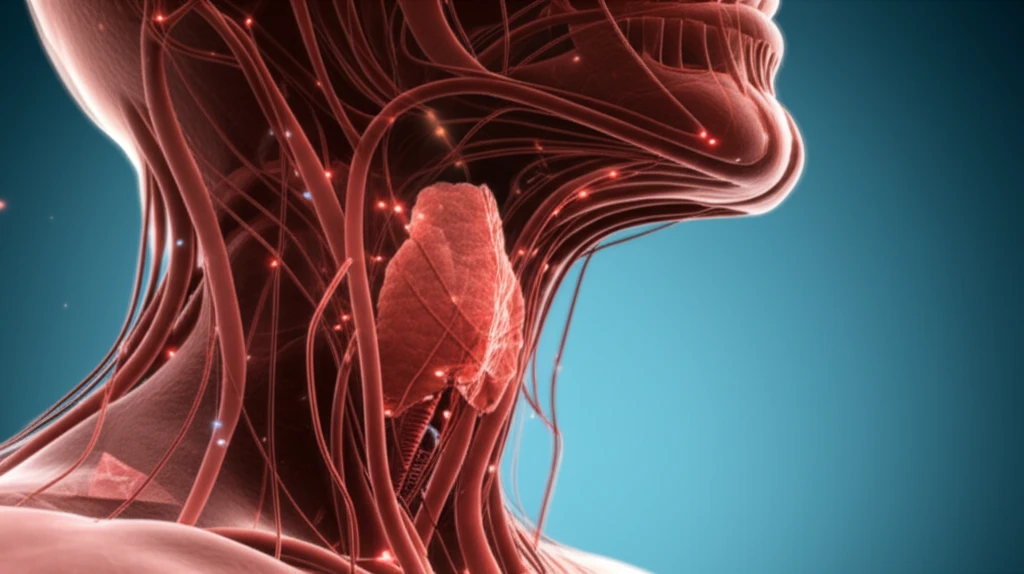
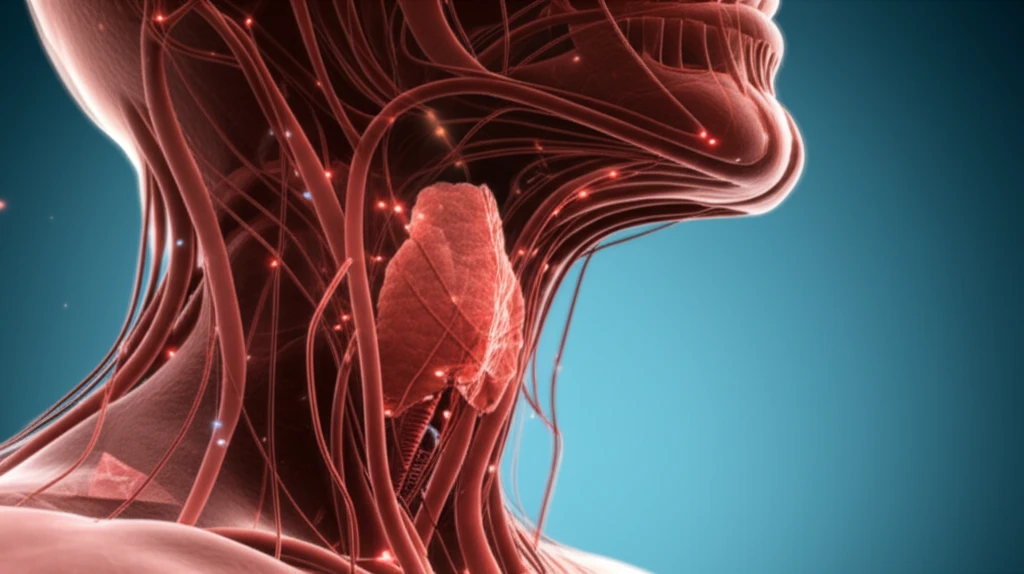
Nasopharyngeal carcinoma (NPC), a type of cancer originating in the upper throat, presents unique challenges due to its hidden location and often late diagnosis. While radiation therapy remains a primary treatment, predicting individual patient outcomes and tailoring treatment plans have been ongoing areas of research.
Recent studies have explored the role of inflammation in cancer progression, leading to the investigation of systemic inflammatory markers found in the blood. These markers, like the neutrophil-to-lymphocyte ratio (NLR) and monocyte-to-lymphocyte ratio (MLR), offer insights into the body's immune response and its impact on tumor behavior.
Now, a new study published in the Journal of Investigative Medicine introduces the Systemic Inflammation Response Index (SIRI) as a promising prognostic marker for NPC. This easily accessible and cost-effective blood test could help doctors better predict patient outcomes and personalize treatment strategies.
Decoding SIRI: A New Tool for Predicting NPC Outcomes
The research team evaluated the prognostic value of SIRI in patients with NPC across two independent groups (primary and validation cohorts). SIRI is calculated using a patient's lymphocyte, neutrophil, and monocyte counts – all standard components of a routine blood test. The study revealed a significant association between SIRI values and overall survival:
- SIRI and Survival: Higher SIRI values correlated with poorer overall survival in both the primary and validation groups.
- Independent Prognostic Value: SIRI was confirmed as an independent predictor of outcomes, offering insights beyond standard clinical assessments.
- Nomogram Integration: A new nomogram combining SIRI and clinicopathological factors was developed to predict patient prognosis effectively.
The Future of NPC Treatment: Personalization Through SIRI
This research underscores the potential of SIRI as a simple, cost-effective tool to refine risk stratification and personalize treatment approaches for patients with NPC. By integrating SIRI into prognostic models, clinicians can gain a more comprehensive understanding of individual patient risk and tailor interventions accordingly.
The study authors emphasize that while these findings are promising, further research is warranted to validate the clinical utility of SIRI in diverse patient populations and treatment settings. Future studies could also explore the underlying biological mechanisms linking SIRI to NPC progression, potentially uncovering new therapeutic targets.
Ultimately, the goal is to move towards more personalized and effective cancer care. SIRI represents a step in this direction, offering a readily accessible tool to improve risk assessment and guide treatment decisions in NPC.
