Can a Brain Signal Really Beat Diabetes? The FGF1 Breakthrough
"New research explores how targeting the brain with FGF1 could revolutionize diabetes treatment, offering hope for lasting remission and insulin independence."
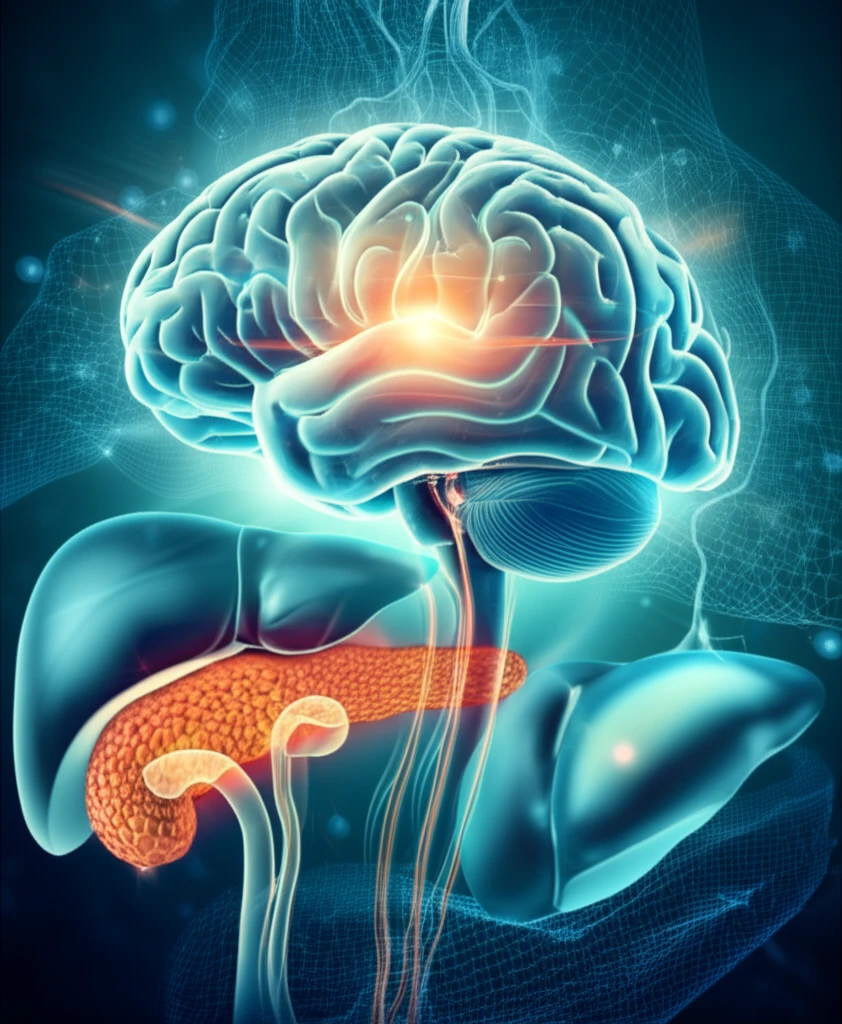
For millions living with type 2 diabetes (T2D), the daily management of blood sugar levels can feel like a never-ending battle. Traditional treatments often involve a combination of medication, diet, and exercise, yet many individuals still struggle to achieve lasting control. But what if the key to unlocking sustained remission lay not in the periphery, but within the intricate network of the brain?
Groundbreaking research is now exploring the potential of fibroblast growth factor 1 (FGF1), delivered directly to the brain, to combat diabetes. This innovative approach, moving beyond conventional methods, aims to tap into the brain’s regulatory mechanisms to achieve enduring anti-diabetic effects. Studies in rodent models have shown remarkable promise, sparking interest in the potential for similar results in humans.
This article dives into the details of this cutting-edge research, examining how FGF1 acts within the brain to improve glucose metabolism, preserve insulin function, and potentially offer a new avenue for managing type 2 diabetes. We'll explore the mechanisms behind this approach, its potential benefits, and what it could mean for the future of diabetes treatment.
How Does FGF1 in the Brain Fight Diabetes?
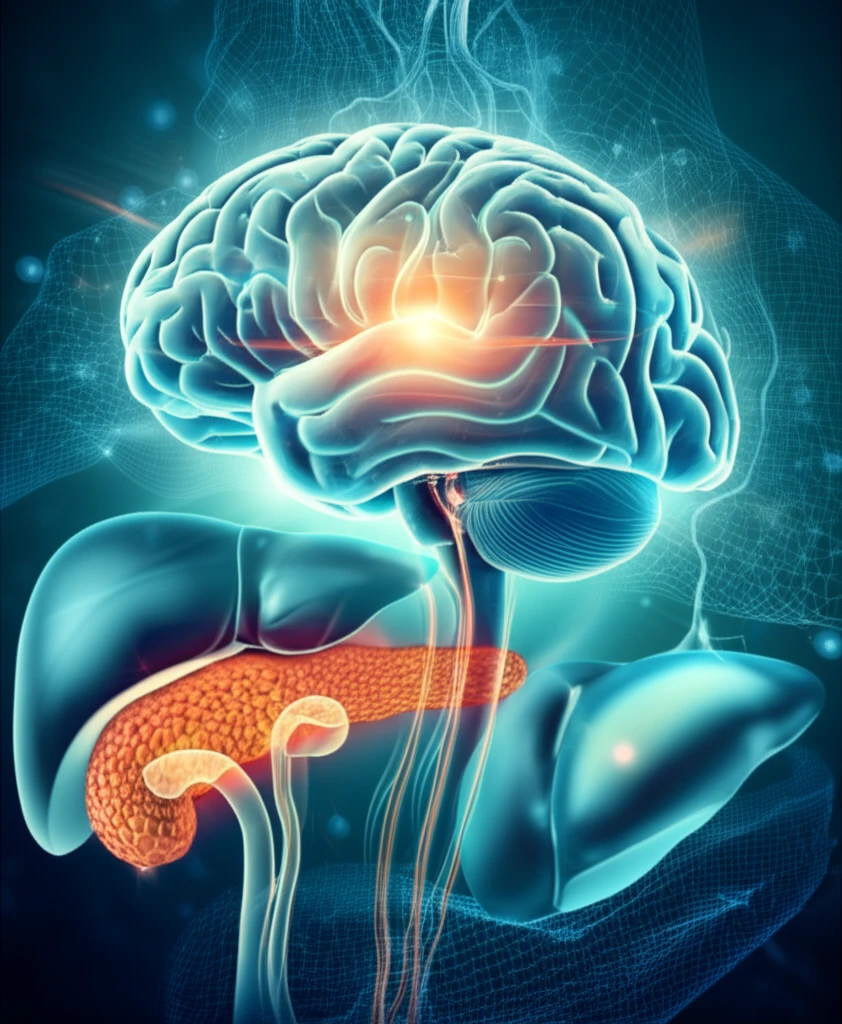
The central idea behind this research is that the brain plays a significant role in regulating glucose metabolism throughout the body. By targeting specific areas of the brain with FGF1, researchers aim to influence these regulatory processes and improve blood sugar control. Here’s a breakdown of the key mechanisms involved:
- Preserving Beta-Cell Function: Type 2 diabetes is often marked by a progressive decline in the function of pancreatic beta-cells, which are responsible for producing insulin. Research suggests that FGF1 can delay this decline, helping to maintain insulin production for a longer period.
- Boosting Hepatic Glucose Uptake: The liver plays a critical role in glucose metabolism, and FGF1 seems to enhance the liver's ability to take up glucose from the bloodstream. This process, known as hepatic glucose uptake (HGU), helps lower blood sugar levels.
- Insulin-Independent Glucose Clearance: Unlike some diabetes medications that rely on increasing insulin secretion or sensitivity, FGF1 appears to promote glucose clearance through mechanisms that don't depend on insulin. This is particularly important for individuals with insulin resistance, a common characteristic of type 2 diabetes.
Looking Ahead: The Future of FGF1 and Diabetes
While the research on FGF1 in the brain is still in its early stages, the findings offer a promising glimpse into the future of diabetes treatment. By targeting the central regulatory mechanisms in the brain, this approach has the potential to overcome some of the limitations of current therapies and offer a more sustainable path towards diabetes remission. As research progresses, it’s important to remember that lifestyle interventions such as diet and exercise remain crucial components of managing diabetes. However, the possibility of a brain-centered treatment adds an exciting new dimension to the fight against this widespread condition.
