Buspirone for IBS Pain: Could This Anxiolytic Be the Answer?
"Unlocking Relief: How Buspirone, traditionally used for anxiety, shows promise in tackling abdominal pain for those with Irritable Bowel Syndrome (IBS)."
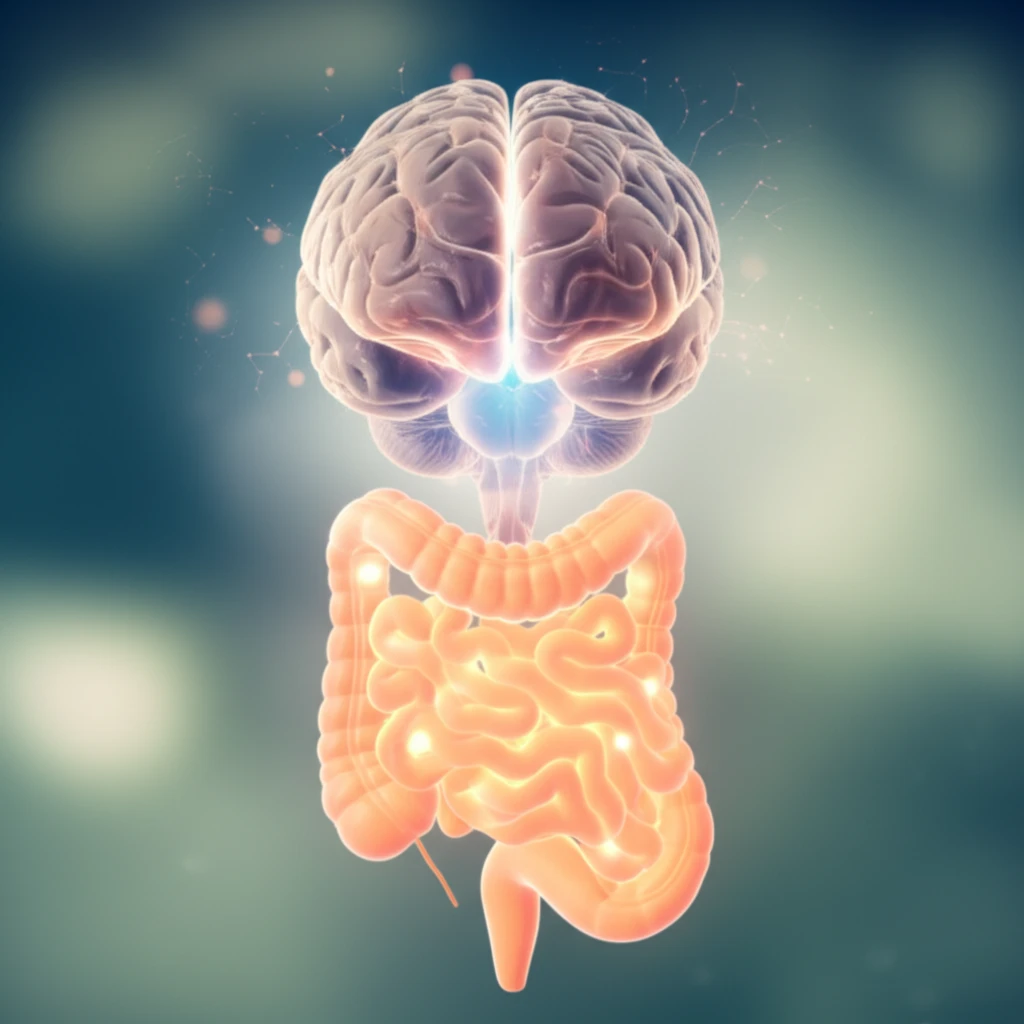
Irritable Bowel Syndrome (IBS) is a widespread gastrointestinal disorder characterized by persistent abdominal pain, bloating, and altered bowel habits. Millions worldwide grapple with the debilitating effects of IBS, often leading to a significant reduction in their quality of life. The quest for effective treatments has been ongoing, with a focus on understanding the intricate relationship between the gut and the brain.
Within this complex interplay, the role of serotonin, a neurotransmitter crucial for both mood regulation and gut function, has gained significant attention. Serotonin receptors, particularly the 5-HT1a receptors, are emerging as key players in modulating pain signals within the gut-brain axis. These receptors are strategically located throughout the body, including the ventrolateral medulla (VLM) in the brain, which plays a critical role in pain processing.
Enter buspirone, an anxiolytic medication commonly prescribed for anxiety disorders. Its unique mechanism of action, involving partial agonism of the 5-HT1a receptors, has sparked interest in its potential beyond mental health. Recent research indicates that buspirone might offer a new avenue for IBS pain relief, prompting a deeper look into how this medication interacts with the complex mechanisms of IBS.
The Brain-Gut Connection: How Buspirone Targets IBS Pain
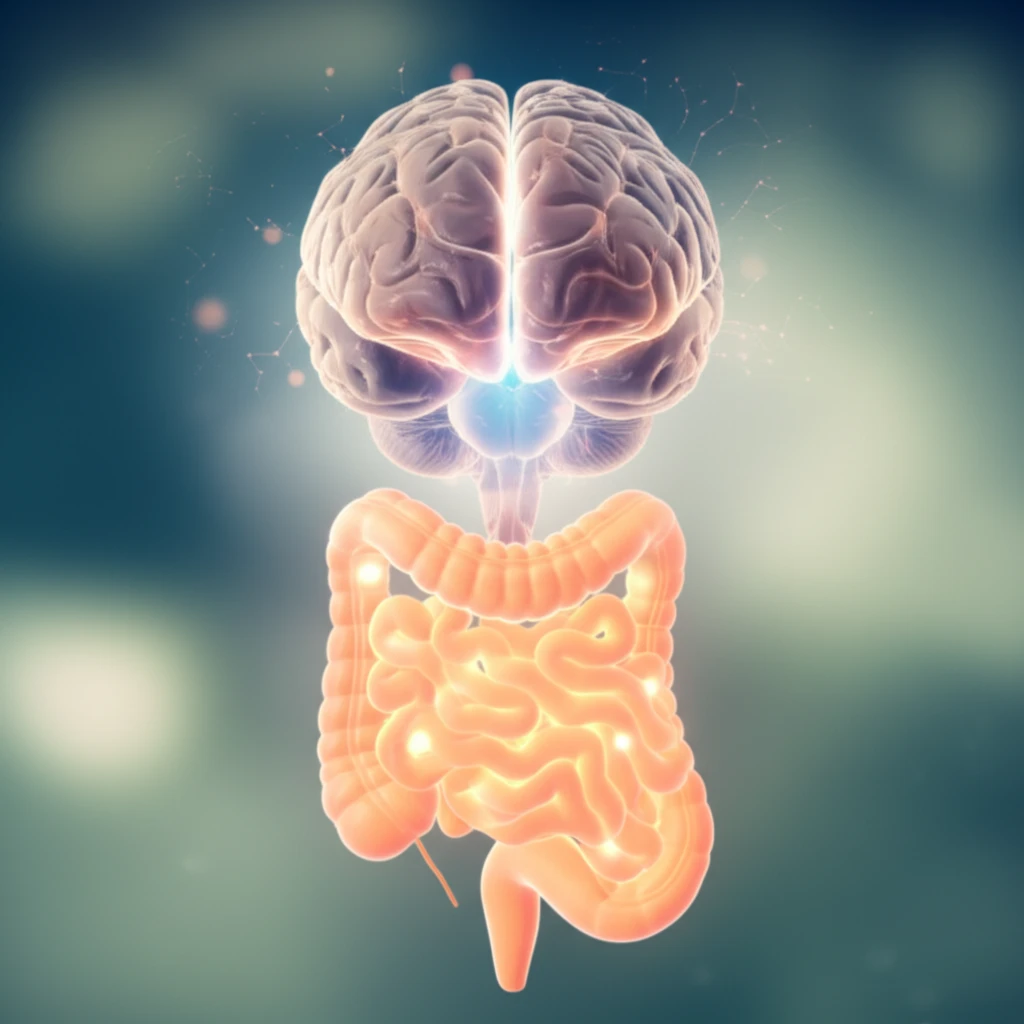
The core of IBS pain often lies in the brain's misinterpretation of signals from the gut. The VLM, a region within the brainstem, acts as a central processing unit for pain signals. When the gut experiences distress, such as the contractions or inflammation, these signals are relayed to the VLM, which then processes and amplifies the pain sensation. The 5-HT1a receptors, abundant in the VLM, provide a potential target for medications aiming to modulate these pain signals.
- Targeted Action: Buspirone specifically interacts with 5-HT1a receptors, minimizing potential side effects compared to broader-acting medications.
- Dual Mechanism: It influences pain perception in both the central nervous system and potentially in the gut itself.
- Pain Signal Modulation: Buspirone can reduce the intensity of pain signals by calming the overactive pain pathways in the brain.
Looking Ahead: The Promise of Buspirone for IBS Pain
While the current research on buspirone for IBS pain is promising, it's essential to approach this information with a balanced perspective. Buspirone is not a cure-all, and its effectiveness may vary among individuals. Further research is needed to determine the optimal dosage, long-term effects, and potential side effects in a larger and more diverse population. However, for those struggling with IBS pain, buspirone represents a potential avenue for relief. By targeting the complex gut-brain connection, buspirone offers a new way to tackle the debilitating symptoms of IBS, providing a beacon of hope in the ongoing quest for effective treatment options.
