Broken Bones, Silent Thief: Could Hyperparathyroidism Be Weakening Your Bones?
"Uncover the link between primary hyperparathyroidism and unexpected fractures, and learn how early screening can safeguard your bone health."
Imagine a seemingly ordinary fall leading to extraordinary consequences: a bilateral hip fracture. This was the reality for an 84-year-old man whose case, detailed in a recent European Geriatric Medicine report, unveiled a surprising connection between bone fragility and an often overlooked endocrine disorder: primary hyperparathyroidism (PHPT). This case underscores the importance of considering underlying conditions when addressing fractures, especially in older adults.
The patient, who had a history of essential hypertension and atrial fibrillation, experienced two falls, each from his own height, resulting in hip contusions. Subsequent examination revealed bilateral subcapital fractures, necessitating admission to the Orthogeriatrics Unit for thorough evaluation and surgical intervention. What initially appeared as a consequence of aging and falls soon revealed a more complex underlying issue.
Beyond the immediate fractures, the man's geriatric assessment highlighted his independent living status and autonomous mobility, aided only by a walking stick outdoors. Cognitive function was intact, suggesting a physically driven cause for his falls. Routine osteoporosis screening, however, revealed significant abnormalities: acute renal failure, elevated calcium levels, markedly elevated parathyroid hormone (PTH), and vitamin D deficiency. These findings pointed towards primary hyperparathyroidism.
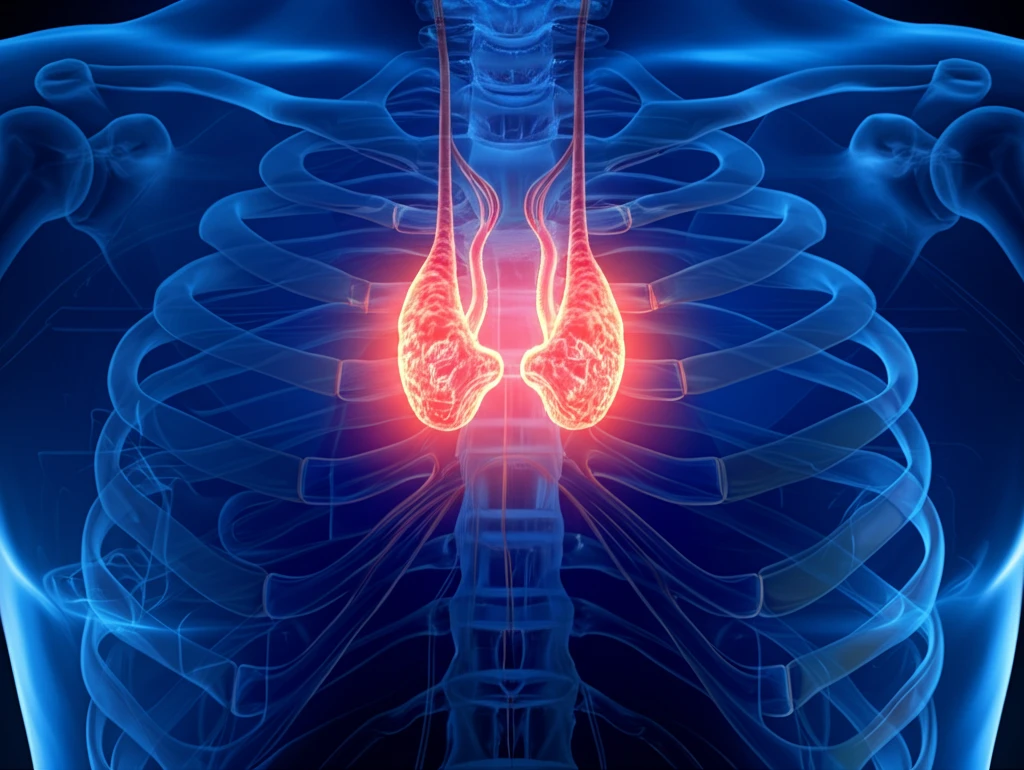
What is Primary Hyperparathyroidism (PHPT) and How Does It Weaken Bones?
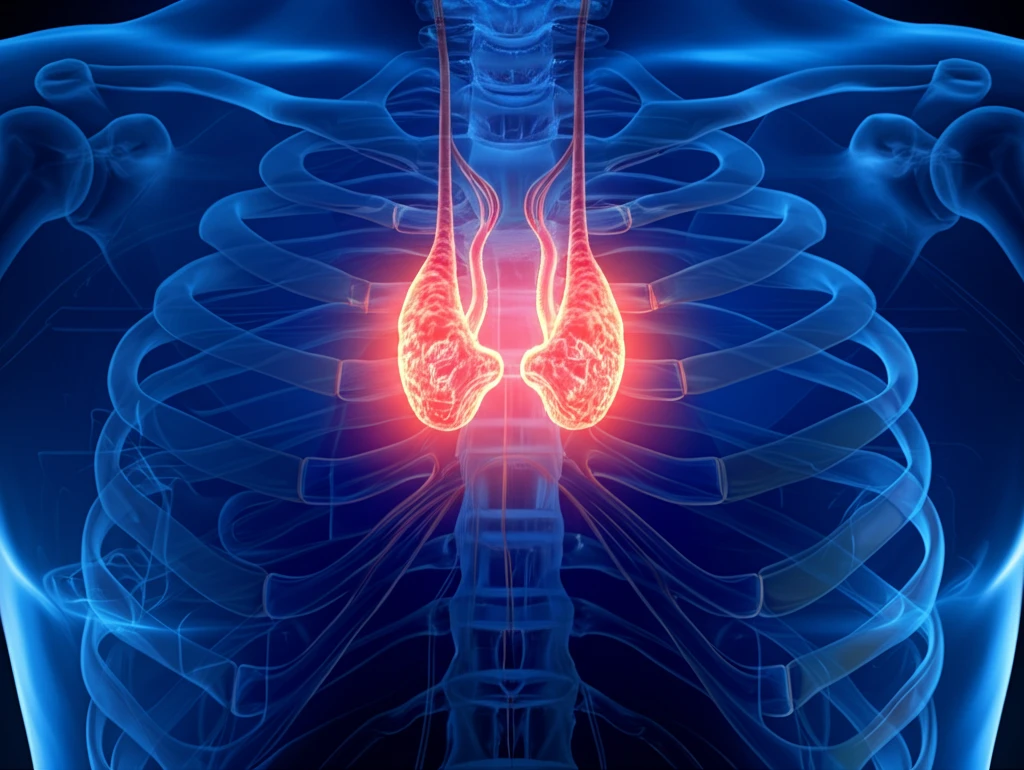
Primary hyperparathyroidism (PHPT) is an endocrine disorder characterized by excessive secretion of parathyroid hormone (PTH) by one or more of the parathyroid glands. This leads to elevated calcium levels in the blood (hypercalcemia). While many individuals with PHPT may experience mild or no symptoms, the chronic elevation of calcium can have significant effects on various organs, most notably the bones and kidneys.
- Increased Bone Resorption: PTH stimulates the breakdown of bone tissue (resorption) to release calcium into the bloodstream, trying to correct the calcium imbalance. Over time, this excessive bone resorption leads to decreased bone density and increased risk of fractures.
- Disrupted Bone Remodeling: Bone is constantly being remodeled, with old bone being removed and new bone being formed. PHPT disrupts this balance, favoring bone resorption over bone formation, leading to weaker, more porous bones.
- Cortical Bone Loss: PHPT primarily affects cortical bone, which is the dense outer layer of bone that provides strength and support. This type of bone loss is particularly detrimental to long bones like the hip, increasing the risk of fractures.
The Takeaway: Don't Ignore the Silent Signs
This case highlights a critical lesson: fractures, especially in older adults, should prompt a thorough investigation for underlying causes like primary hyperparathyroidism. Early diagnosis and appropriate management, including surgical intervention when necessary, are crucial for preventing further bone loss, reducing fracture risk, and improving overall quality of life. Be proactive about your bone health and discuss any concerns with your doctor. Simple screening tests can make a world of difference.
