Breathing Easy: A Safe Approach to Anesthesia with Mediastinal Masses
"How innovative techniques are improving outcomes for patients with airway obstruction."
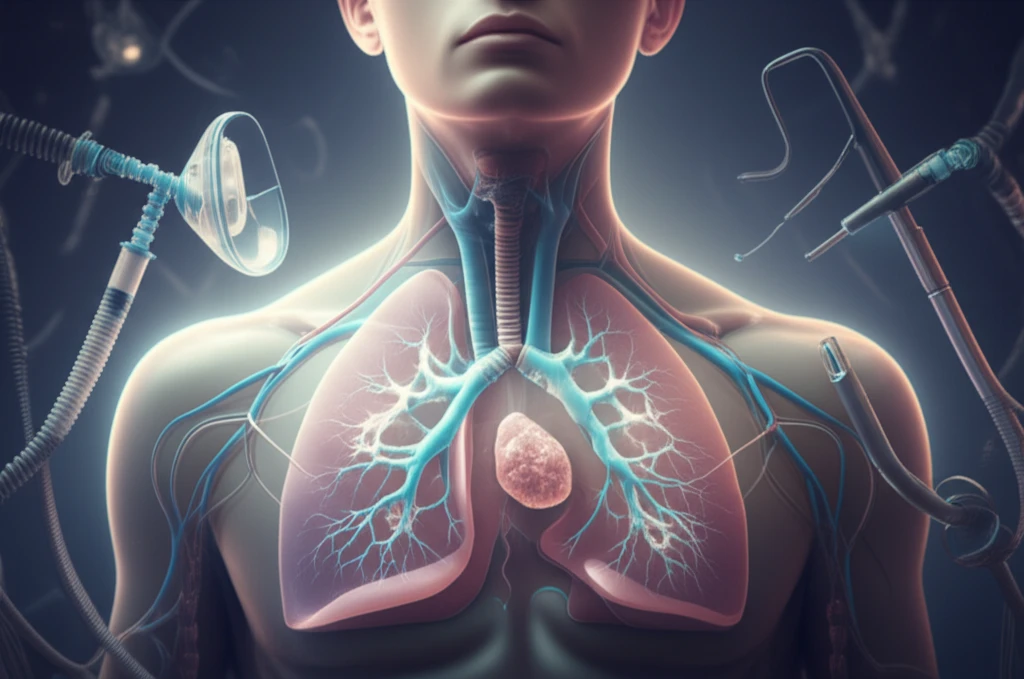
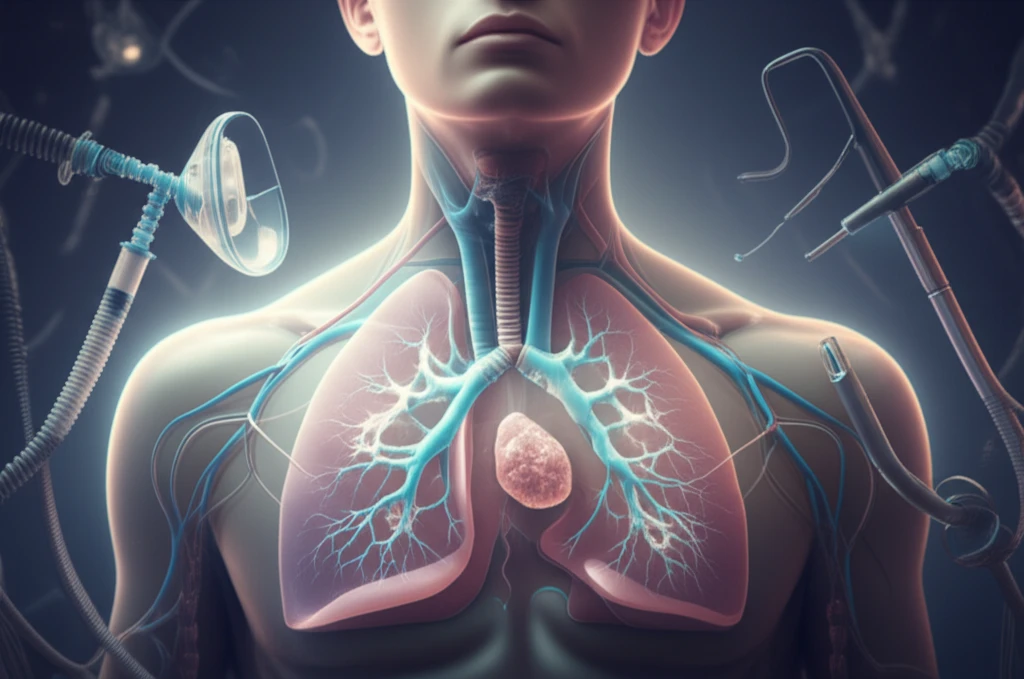
Anterior mediastinal masses, tumors located in the front part of the chest cavity, can pose significant challenges during anesthesia. These masses can compress the trachea (windpipe) and major blood vessels, leading to airway narrowing and cardiovascular complications, especially when muscle relaxants are administered. Traditionally, anesthesiologists have relied on inhalation induction or awake intubation to avoid the risks associated with muscle relaxation.
However, a new approach is emerging that allows for the safe use of muscle relaxants in these complex cases. This technique involves a carefully orchestrated sequence of total intravenous anesthesia (TIVA), tailored positive pressure ventilation, and judicious administration of muscle relaxants. This method aims to maintain stable breathing and circulation while providing optimal conditions for surgical or diagnostic procedures.
This article explores two case reports that highlight the successful application of this innovative approach. By understanding the principles and techniques involved, healthcare professionals can enhance their ability to manage patients with anterior mediastinal masses safely and effectively. This technique minimizes the potential life-threatening complications.
Step-by-Step: How to Safely Induce Anesthesia in Patients with Mediastinal Masses
The following case reports detail the successful anesthetic management of two patients with anterior mediastinal masses using a carefully planned and executed approach. The key steps involve:
- Preoperative Assessment: A comprehensive evaluation to understand the degree of airway and cardiovascular compromise.
- Patient Positioning and Preoxygenation: Positioning the patient upright (sitting position) to maximize lung capacity and preoxygenating with 100% oxygen to build oxygen reserves.
- Total Intravenous Anesthesia (TIVA): Using intravenous medications like propofol and fentanyl to induce anesthesia while carefully monitoring the patient's level of consciousness with a Bispectral Index (BIS) monitor.
- Positive Pressure Ventilation: Initiating gentle positive pressure ventilation as the patient becomes sedated, using appropriate tidal volumes and respiratory rates to avoid air trapping.
- Muscle Relaxation: Administering muscle relaxants (e.g., succinylcholine or cisatracurium) only after ensuring adequate ventilation and hemodynamic stability.
- Bronchoscopic Guidance: Using a rigid bronchoscope to visualize the airway, facilitate intubation, and maintain airway patency.
- Tailored Ventilation Strategies: Adjusting ventilation parameters, such as inspiratory-to-expiratory (I:E) ratio and peak airway pressures, to optimize gas exchange and minimize airway pressure.
Conclusion: A Safer Path Forward
The described cases demonstrate that a carefully planned approach to anesthesia, combining TIVA, tailored positive pressure ventilation, and judicious use of muscle relaxants, can be safe and effective for patients with anterior mediastinal masses. This technique offers several advantages over traditional methods, including improved control of ventilation, better visualization of the airway, and reduced risk of airway collapse. By adopting these strategies, clinicians can enhance patient safety and improve outcomes in this challenging population.
