Breathe Easier: How Emphysema Treatment is Evolving After Lung Cancer Surgery
"Discover how new research is changing the approach to managing emphysema in lung cancer patients post-lobectomy, enhancing recovery and quality of life."
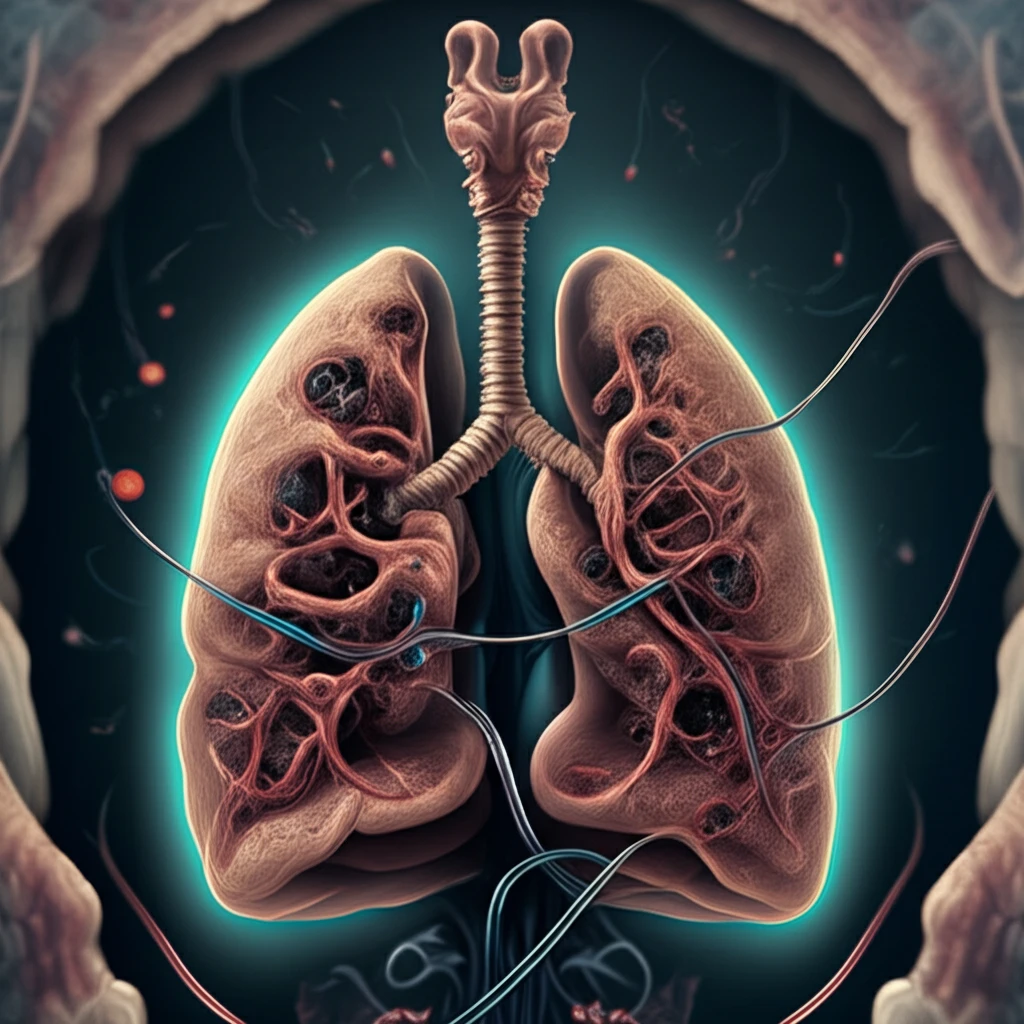
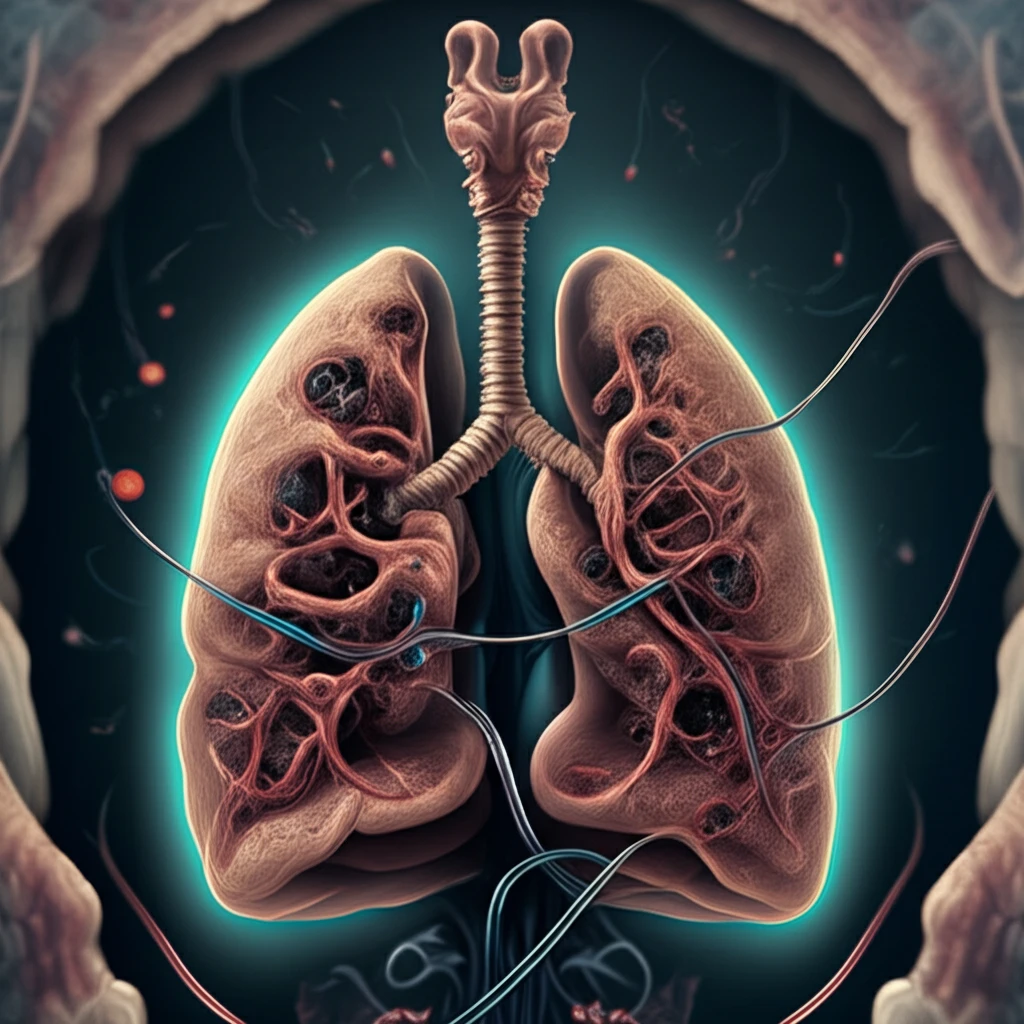
Lung cancer surgery, particularly lobectomy (the removal of a lobe of the lung), is a critical intervention, but it often comes with postoperative challenges. One significant factor influencing recovery is the presence of emphysema, a chronic lung condition characterized by damage to the air sacs in the lungs. Understanding how emphysema affects outcomes after surgery is essential for improving patient care.
Traditionally, post-lobectomy care involves the use of chest tubes to drain fluids and air from the chest cavity, facilitating lung expansion and preventing complications. However, the effectiveness of chest tube management can be significantly influenced by the patient's pre-existing lung conditions, such as emphysema. A recent study published in the Journal of Thoracic Oncology delves into this intersection, providing valuable insights into how emphysema impacts chest tube drainage and overall recovery.
This article explores the findings of the study, focusing on how quantitative assessments of emphysema can help tailor postoperative care, reduce prolonged air leaks, and improve patient outcomes following lung cancer surgery. We will break down the key findings, discuss the implications for medical professionals, and offer a patient-friendly perspective on managing emphysema in the context of lung cancer treatment.
Emphysema's Impact on Post-Lobectomy Recovery: What the Research Shows
A study was conducted to evaluate the effect of emphysema on chest tube drainage following lobectomy for non-small cell lung cancer (NSCLC). The research, published in the Journal of Thoracic Oncology, employed a prospective, randomized trial design involving patients undergoing lobectomy between February 2016 and December 2017. The study aimed to determine whether using one chest tube versus two chest tubes could optimize drainage and reduce complications based on the severity of emphysema.
- Patient Randomization: Patients were randomized in a 1:1 ratio to either a single chest tube group or a two chest tube group at the end of the operation.
- Suction Management: Controlled suction of -20 cm H2O was applied on the day of surgery, which was then switched to -8 cm H2O on the first postoperative day.
- Data Collection: Researchers recorded the amount and duration of air leak, chest tube output, and differential pleural pressure. Digital chest drainage systems were used to monitor pressure.
- Emphysema Quantification: Quantitative analysis of emphysema was performed using the syngo CT. 3D Pulmo software to assess the extent and severity of emphysema in each patient.
- Prolonged Air Leak Definition: Air leak lasting more than 72 hours was defined as a prolonged air leak. Chest tubes were removed when there was no air leak for more than 24 hours, and the chest tube output was less than 250 mL/day.
Moving Forward: Better Postoperative Care for Lung Cancer Patients
The findings from this research emphasize the importance of quantitatively assessing emphysema in patients undergoing lobectomy for NSCLC. By understanding the extent of emphysema, medical teams can make more informed decisions about chest tube management, potentially reducing complications such as prolonged air leaks. This personalized approach can lead to improved patient outcomes, shorter hospital stays, and enhanced quality of life for individuals recovering from lung cancer surgery.
