Brain AVM Embolization: A Comprehensive Guide to Transvenous Techniques
"Discover how transvenous embolization is revolutionizing the treatment of brain arteriovenous malformations, offering new hope for patients seeking minimally invasive solutions."
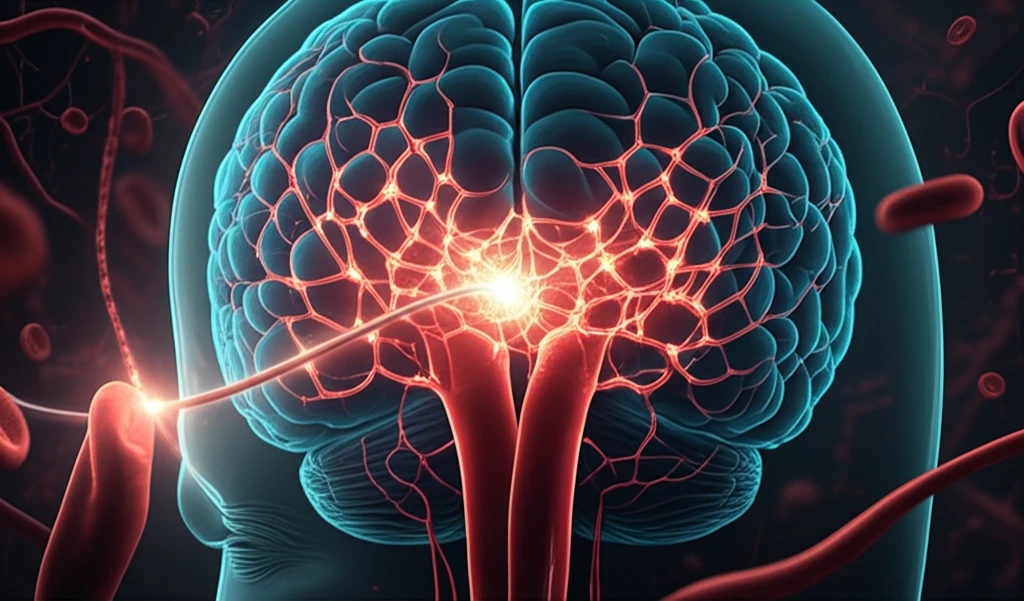
Brain arteriovenous malformations (AVMs) present a significant challenge in neurosurgery. These abnormal tangles of blood vessels can disrupt normal blood flow and lead to serious complications, including hemorrhage, seizures, and neurological deficits. Traditional treatment approaches have included surgical resection, stereotactic radiosurgery, and transarterial embolization. However, the emergence of transvenous embolization is now providing a new avenue for treating these complex vascular lesions.
Transvenous embolization involves navigating a catheter through the veins to access and occlude the AVM directly. This approach offers several potential advantages over traditional methods, particularly for AVMs located in deep or difficult-to-reach areas of the brain. By targeting the AVM through the venous system, neurointerventionalists can often achieve complete obliteration of the malformation while minimizing the risk of damage to surrounding healthy tissue.
This article delves into the details of transvenous embolization for brain AVMs, exploring its indications, techniques, outcomes, and potential complications. Whether you're a healthcare professional seeking to expand your knowledge or a patient exploring treatment options, this guide provides a comprehensive overview of this innovative approach.
What Makes Transvenous Embolization a Game-Changer for Brain AVMs?
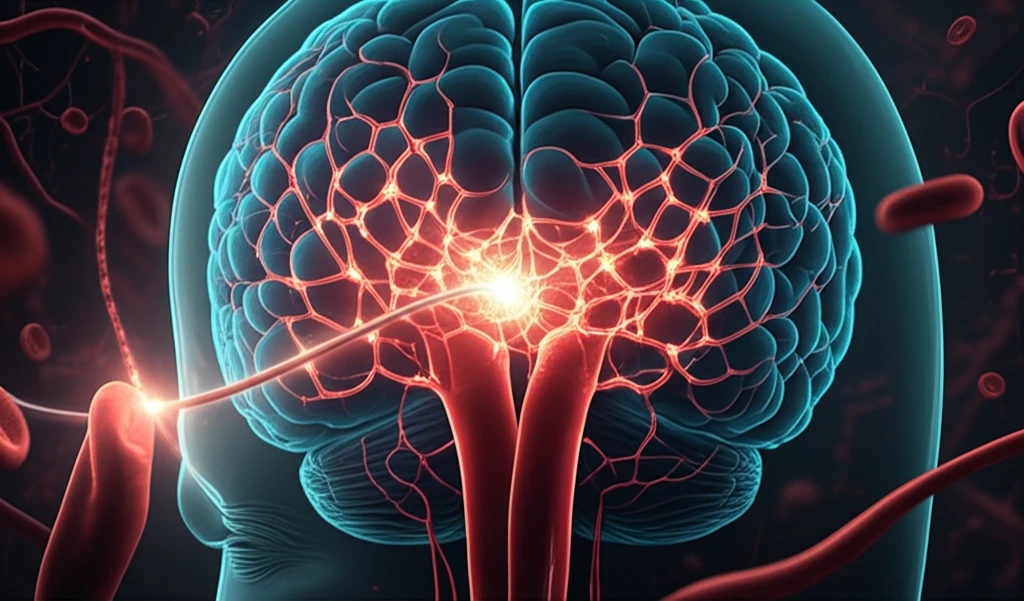
Transvenous embolization is rapidly gaining traction as a valuable tool in the treatment of brain AVMs due to its unique advantages. This minimally invasive technique allows neurointerventionalists to access AVMs that may be challenging or impossible to reach via traditional transarterial approaches or open surgery. By navigating through the venous system, clinicians can directly target the AVM nidus, the core of the malformation, and deliver embolic agents to occlude it.
- Accessibility: Reaching deep-seated AVMs that are otherwise inaccessible.
- Precision: Direct targeting of the AVM nidus for effective occlusion.
- Minimally Invasive: Reduced risk of damage to surrounding brain tissue.
- High Obliteration Rates: Studies show excellent rates of complete AVM obliteration.
- Reduced Complications: Lower incidence of certain complications compared to other methods.
The Future of AVM Treatment: Transvenous Embolization and Beyond
Transvenous embolization represents a significant step forward in the treatment of brain AVMs. As technology advances and techniques are refined, this approach is poised to play an increasingly important role in neurovascular care. Ongoing research is focused on optimizing embolic agents, improving catheter navigation, and identifying the ideal candidates for this innovative procedure. By continuing to push the boundaries of what's possible, neurointerventionalists are paving the way for safer, more effective treatments and improved outcomes for patients with brain AVMs.
