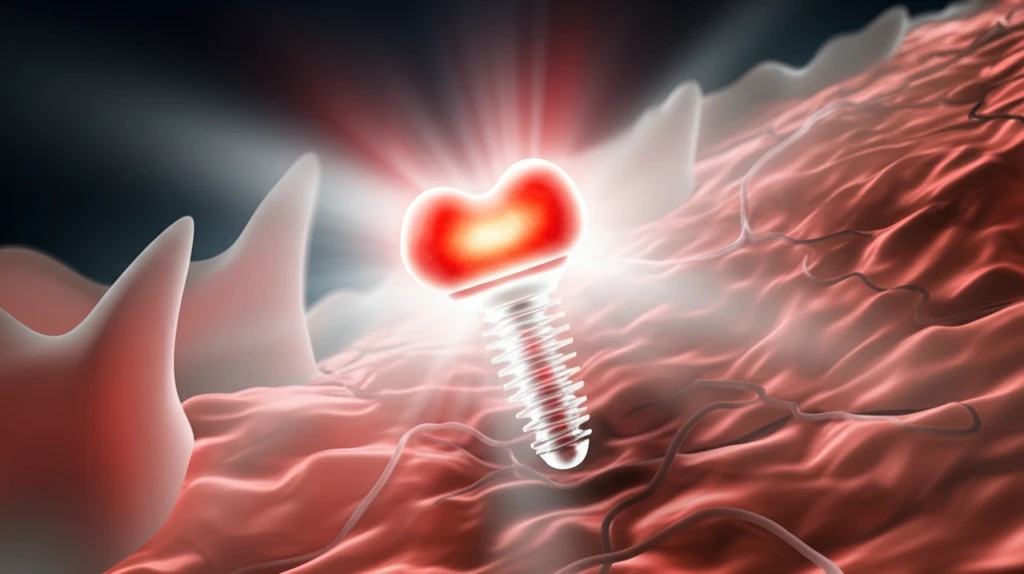
Bone Implants Reimagined: How Red Phosphorus and Light Could Revolutionize Orthopedics
"Discover the cutting-edge research exploring how red phosphorus and near-infrared light are creating antibacterial, bone-healing implants for a future free of infection and repeat surgeries."
For decades, artificial bone implants have been a cornerstone of fracture fixation, dental procedures, and orthopedic surgeries. Yet, despite advancements in biomaterials, a persistent challenge remains: implant-associated infections (IAIs). These infections not only cause significant distress to patients but often necessitate repeated surgeries and incur substantial healthcare costs.
Traditional strategies to combat IAIs include designing materials that disrupt biofilm formation or engineering surfaces with anti-infective and immuno-enhancing properties. However, a promising new avenue involves photothermal therapy (PTT) and photodynamic therapy (PDT) using near-infrared (NIR) light. These therapies leverage light to kill bacteria with fewer side effects and deeper tissue penetration.
Now, researchers are exploring the potential of red phosphorus, a biocompatible material with remarkable photothermal capabilities, combined with NIR light to create a new generation of bone implants. This innovative approach aims to tackle infections and promote bone regeneration, offering a beacon of hope for patients seeking improved orthopedic outcomes.
Red Phosphorus and Near-Infrared Light: A Powerful Partnership for Bone Implants
The core innovation lies in the combination of red phosphorus (RP) and near-infrared (NIR) light. Red phosphorus, a nontoxic allotrope of phosphorus, exhibits excellent biocompatibility and efficient photothermal capabilities. When exposed to NIR light, RP converts light energy into heat, creating a localized hyperthermia effect that can eradicate bacteria. This approach is particularly attractive because RP is significantly cheaper than other alternatives like black phosphorus.
- Photothermal Therapy (PTT): Red phosphorus converts NIR light into heat, killing bacteria.
- Photodynamic Therapy (PDT): IR780 generates reactive oxygen species (ROS), further damaging bacterial cells.
- Osteogenesis: RGDC promotes bone regeneration, ensuring the implant integrates seamlessly with the surrounding tissue.
Future Directions and Clinical Implications
The development of Ti-RP-IR780-RGDC bone implants represents a significant step forward in orthopedic biomaterials. Its ability to combat infections and promote bone regeneration holds great promise for improving patient outcomes and reducing the burden of revision surgeries. As research progresses, future studies should focus on long-term biocompatibility, optimizing the delivery of NIR light, and conducting clinical trials to validate the effectiveness of this innovative approach in human subjects. This could revolutionize orthopedic practices, providing clinicians with a powerful tool to enhance bone healing and minimize post-operative complications.
