Blood Transfusions After TAVI: Are They Putting Your Heart at Risk?
"Unraveling the Link Between Blood Transfusions and Long-Term Mortality in Patients Undergoing Transcatheter Aortic Valve Implantation"
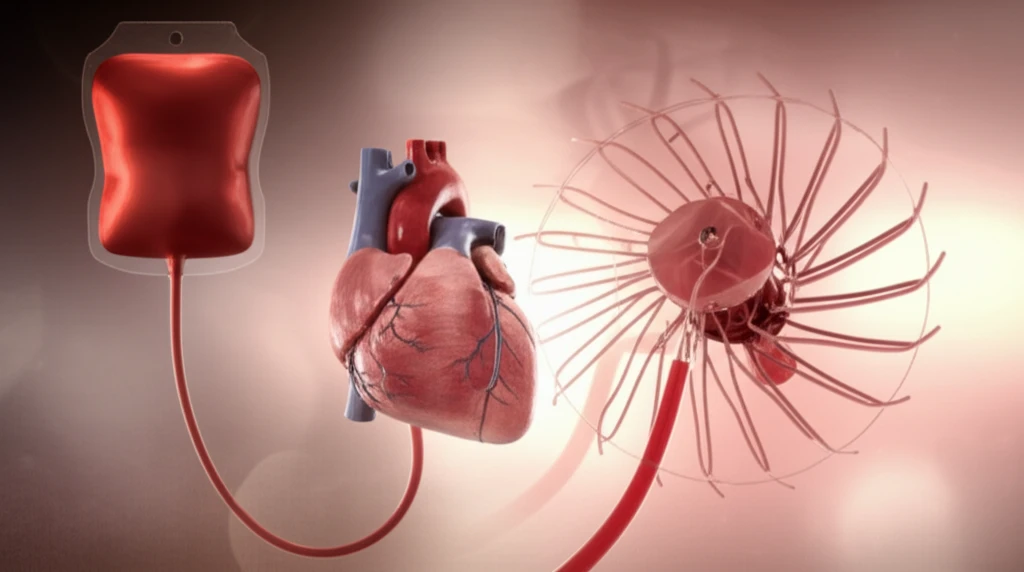
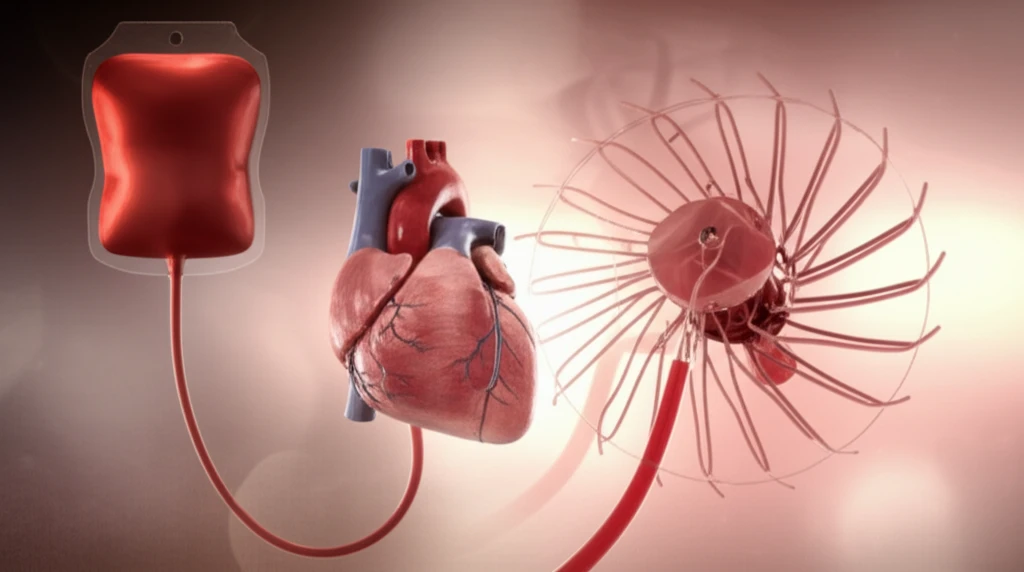
Transcatheter Aortic Valve Implantation (TAVI) has revolutionized the treatment of severe aortic stenosis, offering a less invasive option for many. Yet, as with any medical procedure, understanding the potential risks and complications is paramount. Recent research has shed light on a critical factor impacting patient outcomes: blood transfusions. This article explores the findings, providing a comprehensive overview of the relationship between blood transfusions and long-term mortality following TAVI.
The study, published in the International Heart Journal, investigated the association between blood transfusions and 12-month mortality in patients who underwent TAVI. The results reveal a significant link between the need for blood transfusions during or after the procedure and an increased risk of adverse outcomes. This information is crucial for both patients considering TAVI and healthcare providers striving to optimize patient care.
This article aims to break down the complex findings of the study, providing clear, actionable insights. We'll explore the impact of blood transfusions on patient outcomes, discuss the implications for clinical practice, and offer a better understanding of how these insights can improve the lives of those undergoing TAVI.
The Study: Unveiling the Risks of Blood Transfusions After TAVI
The research, conducted on a cohort of 101 patients with severe aortic stenosis, focused on the outcomes following TAVI. Patients were carefully monitored, and data was collected on various factors, including the need for blood transfusions, complications, and mortality rates. The study's methodology involved a detailed analysis of patient characteristics, procedural details, and follow-up outcomes.
- Increased Mortality: The study revealed that patients who received blood transfusions had a significantly higher 12-month all-cause mortality rate compared to those who did not.
- Predictive Factor: Blood transfusion was identified as an independent predictor of increased mortality, even after adjusting for other factors.
- Prolonged Hospital Stay: Patients requiring transfusions also experienced longer hospital stays, indicating a more complex recovery process.
Moving Forward: Implications and Future Directions
The study's findings offer valuable insights for patients and healthcare professionals. For patients, understanding the risks associated with blood transfusions can help inform decision-making and promote a proactive approach to recovery. For healthcare providers, the research highlights the importance of careful patient selection, meticulous procedural techniques, and effective management of bleeding complications. Further research is needed to explore strategies for minimizing the need for blood transfusions and improving outcomes for patients undergoing TAVI. These could include exploring alternative antiplatelet regimens or refining techniques to reduce bleeding risks. With continued research and a focus on patient-centered care, we can strive to improve the lives of those affected by aortic stenosis.
