Bile Duct Cancer Breakthroughs: New Insights into Surgical Success
"Surgical strategies for perihilar cholangiocarcinoma and extrahepatic cholangiocarcinoma are evolving. Discover the latest research impacting treatment decisions."
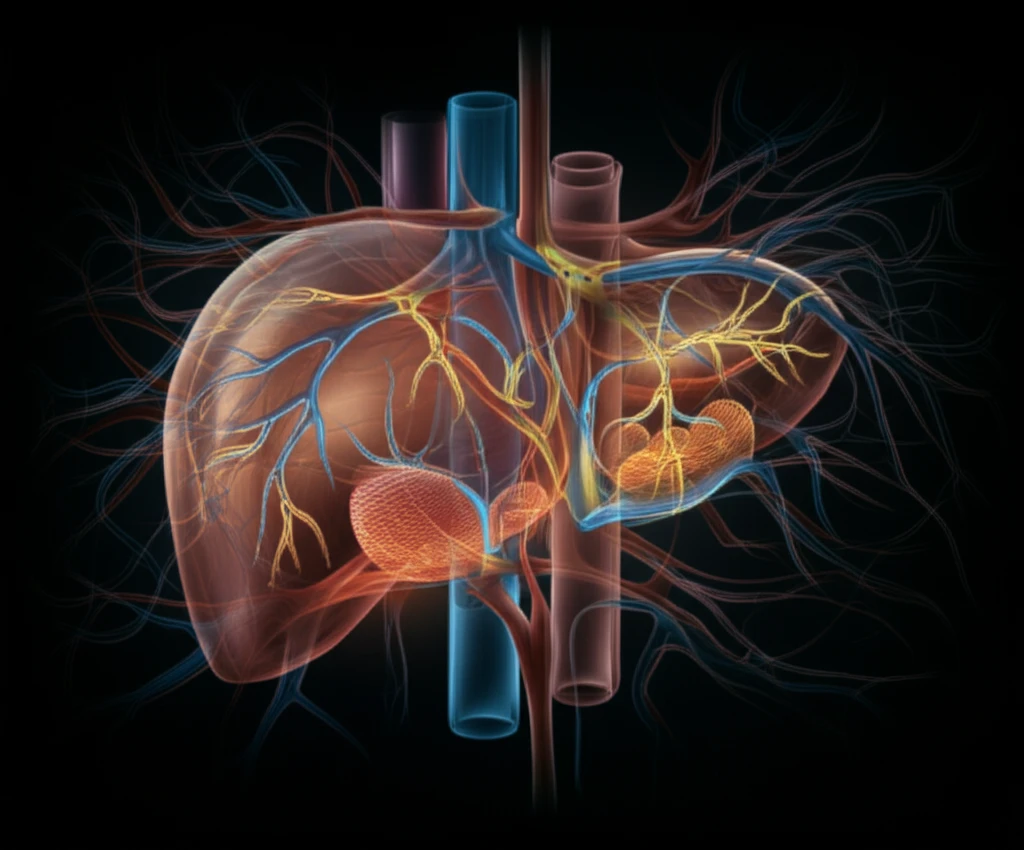
Bile duct cancers, including perihilar cholangiocarcinoma (PHCC) and intrahepatic cholangiocarcinoma (IHCC), present significant challenges in treatment. Despite advancements in surgical techniques, long-term survival rates remain lower than many other solid tumors. Researchers are actively working to identify factors that predict successful surgical outcomes and to refine surgical approaches for these complex cancers.
Two recent studies offer valuable insights into improving surgical strategies for bile duct cancer. The first study focuses on developing a preoperative prognostic model for predicting surgical success in patients with perihilar cholangiocarcinoma (PHC). The second study compares the effectiveness of segmental resection (SR) versus pancreaticoduodenectomy (PD) for treating extrahepatic cholangiocarcinoma (EHCC).
This article breaks down the key findings of these studies, explaining how they can potentially impact treatment decisions and improve outcomes for patients facing these challenging diagnoses. We'll explore the factors that contribute to surgical success in PHC and the comparative benefits of different surgical approaches for EHCC.
Predicting Surgical Success in Perihilar Cholangiocarcinoma (PHC)
A multi-center study involving 671 PHC patients who underwent exploratory laparotomy aimed to develop a model for predicting surgical success. Surgical success was defined as complete (R0) resection without 90-day mortality. The study identified several preoperative factors that significantly impacted the likelihood of successful surgery.
- Older age
- Preoperative cholangitis (bile duct infection)
- Involvement of the hepatic artery (the main artery supplying the liver) on imaging
- Suspicious lymph nodes
- Advanced Blumgart stage (a classification system for PHC based on the extent of the tumor)
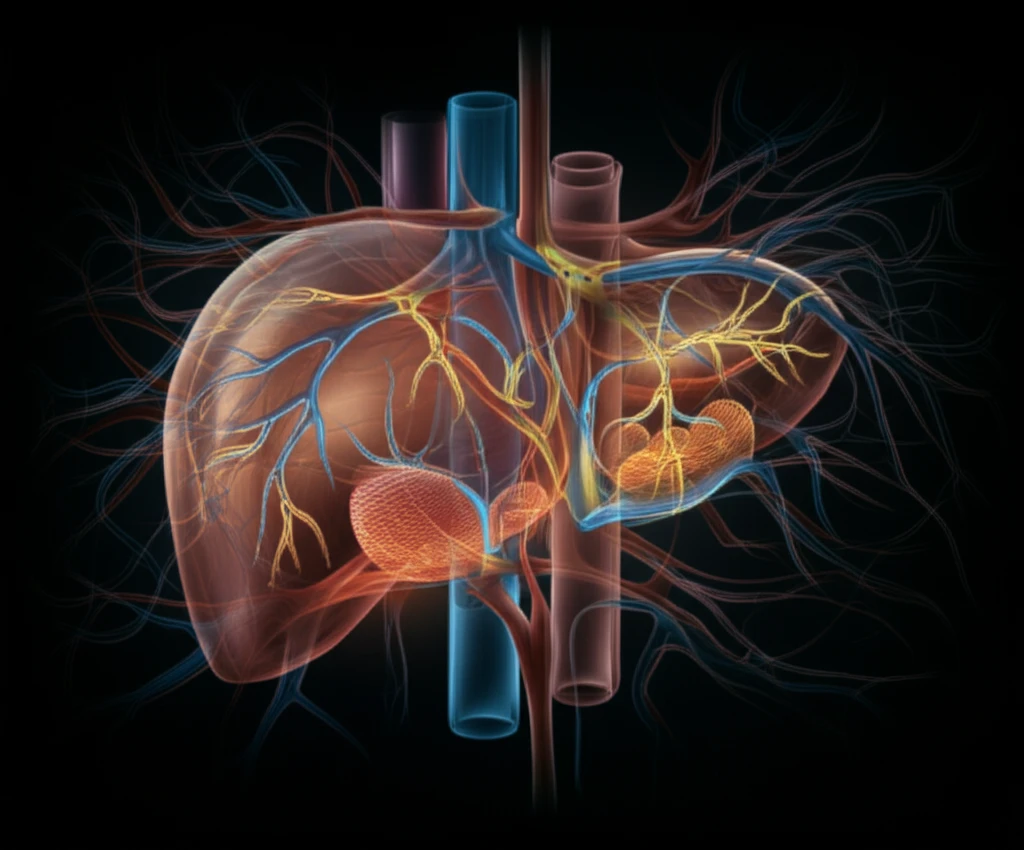
Segmental Resection vs. Pancreaticoduodenectomy for Extrahepatic Cholangiocarcinoma (EHCC)
The second study addressed the question of optimal surgical approach for extrahepatic cholangiocarcinoma (EHCC). Researchers compared segmental resection (SR) with pancreaticoduodenectomy (PD) using a propensity-score matching analysis to minimize bias. The study included 403 patients who underwent R0 resection for EHCC; after matching, 82 patients in each group (SR and PD) were compared.
The results of the study indicated that segmental resection and pancreaticoduodenectomy yielded comparable long-term outcomes in carefully selected patients. This suggests that segmental resection may be a sufficient treatment option for EHCC in certain cases, potentially minimizing the extent of surgery and associated complications. However, patient selection remains crucial to achieving favorable outcomes.
Both studies contribute valuable information to the ongoing effort to improve surgical outcomes for patients with bile duct cancers. The prognostic model for PHC can aid in patient selection and informed decision-making, while the comparison of surgical approaches for EHCC provides evidence to guide treatment strategies. Further research is needed to refine these approaches and personalize treatment plans for individual patients.
