Beyond the Scalpel: Revolutionizing Shoulder Surgery with the 'Dry Catheter' Technique
"A New Approach to Pain Management and Nerve Protection in Shoulder Arthroplasty"
Shoulder surgery, particularly shoulder arthroplasty, is a common procedure aimed at restoring function and alleviating pain. However, like any surgical intervention, it comes with its share of challenges, including managing postoperative pain and the potential for nerve-related complications. Traditionally, interscalene regional anesthesia has been a mainstay for pain control in these procedures. This method, while effective, isn't without risks.
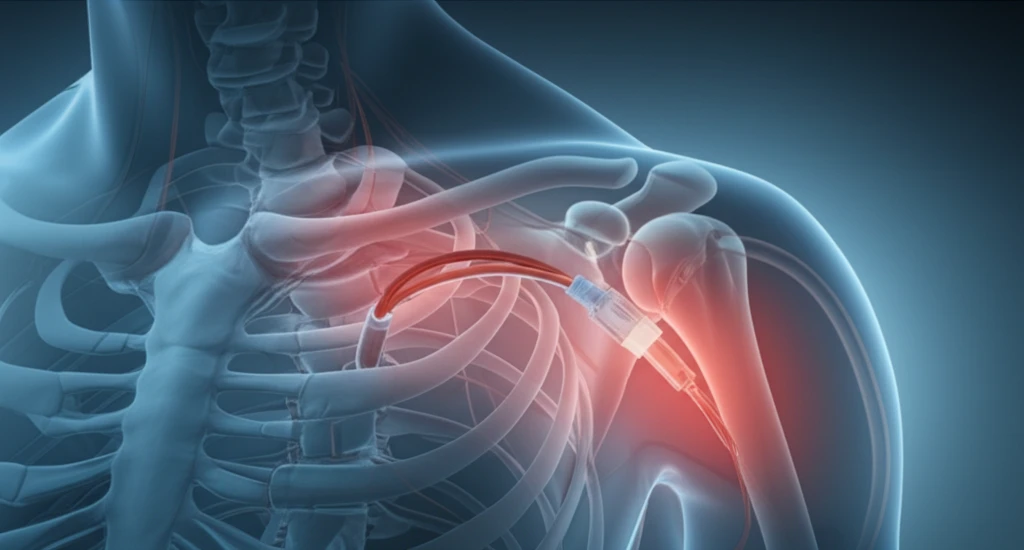
The 'dry catheter' technique emerges as a promising alternative, designed to address these challenges head-on. This innovative approach involves placing, but not activating, a regional anesthetic catheter before surgery. After the procedure, medical professionals conduct a thorough neurovascular examination, and if the examination is normal, the anesthesia is then initiated. This process allows for a more precise evaluation of potential nerve issues, separating surgical complications from those related to anesthesia.
In this article, we will explore the 'dry catheter' technique in detail, including its methodology, advantages, and the impact on patient outcomes. We'll examine how it can help differentiate between surgical complications and those caused by regional anesthesia, offering improved patient care. Our focus is on providing clear, accessible information that will benefit anyone curious about modern shoulder surgery.
Understanding the 'Dry Catheter' Technique: A Step-by-Step Guide
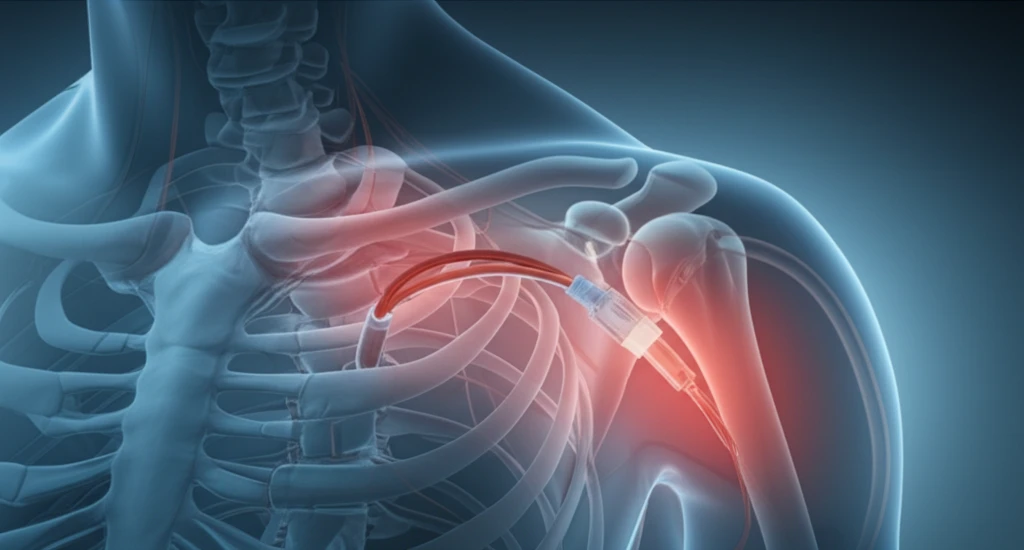
The core of the 'dry catheter' technique lies in its careful, staged approach. The process starts by placing an interscalene catheter before surgery, a standard procedure in regional anesthesia. However, unlike traditional methods, the anesthetic is not administered at this stage. This unique aspect is what sets the technique apart.
- Catheter Placement: An interscalene catheter is positioned before surgery but is not initially activated.
- Post-Surgery Examination: A thorough neurovascular assessment is conducted in the recovery room.
- Anesthesia Initiation: If the neurovascular examination is normal, regional anesthesia is initiated.
- Pain Management: Patients receive pain relief via the regional catheter, adjusted as needed.
The Future of Shoulder Surgery: Innovation in Pain Management
The 'dry catheter' technique represents a significant advancement in shoulder surgery, offering a dual benefit of improved pain management and the ability to accurately identify and address nerve-related complications. As we continue to refine our surgical approaches, innovative techniques like this will undoubtedly play a crucial role in enhancing patient outcomes and the overall quality of care. This method exemplifies the ongoing dedication to surgical precision and patient-centered care.
