Beyond the Needle: How Epidural Therapy is Revolutionizing Chronic Pain Management
"Unlocking Relief: A Groundbreaking Study Reveals the Potential of Epidural Therapy for Chronic Neuropathic Pain"
Chronic pain, a relentless adversary, affects millions worldwide, often leaving individuals trapped in a cycle of suffering. For those grappling with neuropathic pain, a condition stemming from nerve damage, the struggle is particularly acute. Traditional treatments often fall short, leaving patients searching for effective relief. But what if a revolutionary approach, combining the precision of modern medicine with the body's innate healing abilities, held the key?
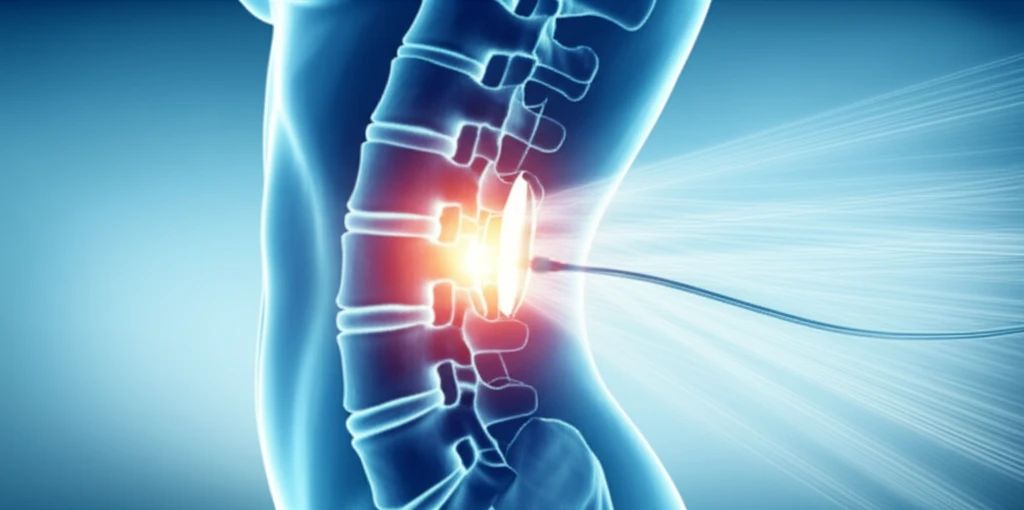
Recent research published in the Journal of Pain Research sheds light on a promising avenue: combined epidural therapy. This innovative treatment, involving the precise delivery of medications directly to the spinal area, offers a beacon of hope for those whose lives have been overshadowed by chronic pain. This article unveils the groundbreaking findings, exploring the science behind the treatment, its potential benefits, and what it means for the future of pain management.
The study, conducted by researchers at the Santa Maria Maddalena Hospital in Italy, focuses on the use of epidural morphine and bupivacaine to treat lumbosacral radicular neuropathic pain. This approach, designed to target the source of the pain, has the potential to offer lasting relief where other treatments have failed. We'll explore the study's methodology, its remarkable results, and the implications for patients and healthcare professionals alike.
Understanding the Science: How Epidural Therapy Works
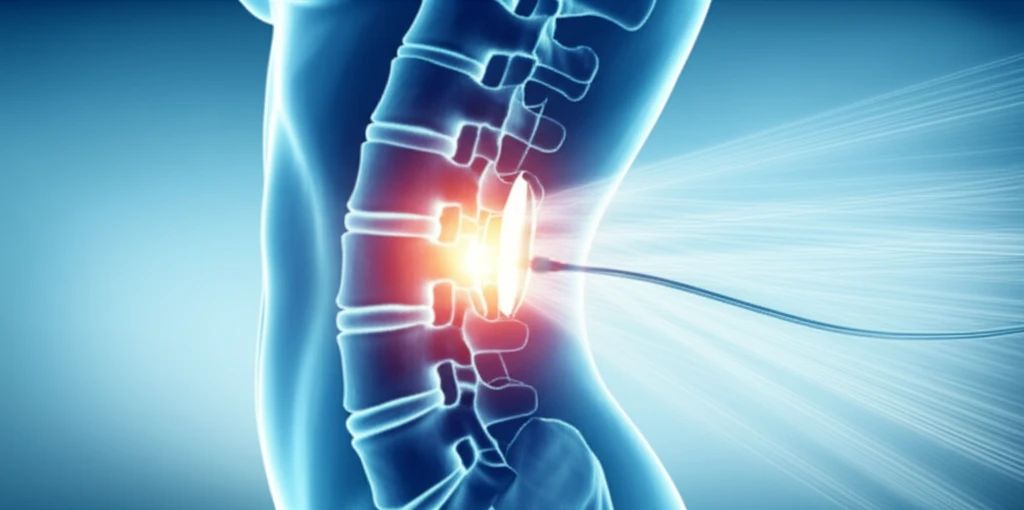
To understand the significance of this study, it's crucial to grasp the underlying principles of epidural therapy. Unlike oral medications that must navigate the body's complex systems, epidural therapy delivers drugs directly to the spinal area. This targeted approach allows for lower doses, minimizing side effects while maximizing effectiveness.
- Targeted Delivery: Drugs are delivered directly to the source of the pain, offering efficient relief.
- Reduced Dosage: Lower doses of medication mean fewer side effects.
- Synergistic Action: Morphine and bupivacaine work together, enhancing pain relief.
- Sustained Relief: The epidural approach can provide sustained pain relief, improving quality of life.
A Brighter Future for Chronic Pain Sufferers
The findings of this study offer more than just a new treatment; they offer a renewed sense of hope. By demonstrating the efficacy of epidural therapy in managing chronic neuropathic pain, the researchers have opened doors for future studies and advancements in pain management. This research underscores the importance of exploring innovative approaches to alleviate the burden of chronic pain and improve the quality of life for countless individuals. As we move forward, this research serves as a reminder of the power of scientific inquiry and the ongoing quest for more effective and compassionate care.
