BCG vs. Chemohyperthermia: A Deep Dive into Bladder Cancer Treatment
"Understanding the Battle: Comparing BCG Instillation and Chemohyperthermia for High-Risk Non-Muscle-Invasive Bladder Cancer"
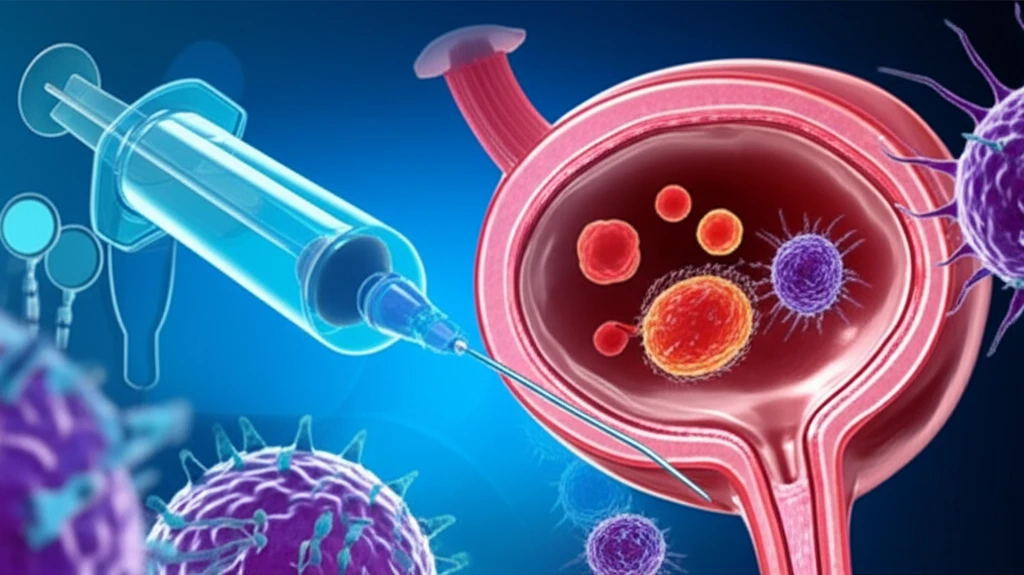
Bladder cancer is a significant health concern, affecting thousands of people worldwide. While the disease is often treatable, the recurrence rate can be high, especially for those with high-risk, non-muscle-invasive bladder cancer (NMIBC). This article delves into two primary treatment options for this type of cancer: bacillus Calmette-Guérin (BCG) instillation and chemohyperthermia (C-HT).
BCG instillation, a form of immunotherapy, has long been a standard treatment for NMIBC. However, chemohyperthermia, which combines chemotherapy with heat, is an emerging alternative. This article will compare these two treatments, examining their effectiveness, benefits, and potential drawbacks, to provide a comprehensive understanding of the latest approaches in bladder cancer care.
The information presented is based on a detailed analysis of research comparing BCG and chemohyperthermia, using a propensity score-matched study to evaluate their efficacy. By understanding these treatment options, patients and their families can make informed decisions and work with their healthcare providers to achieve the best possible outcomes.
BCG vs. Chemohyperthermia: Unveiling the Key Differences
The study, which included a large cohort of patients, provides a detailed comparison of BCG instillation and chemohyperthermia. BCG instillation involves introducing a weakened form of the bacterium Mycobacterium bovis into the bladder, stimulating the immune system to attack cancer cells. Chemohyperthermia, on the other hand, combines chemotherapy drugs, such as mitomycin-C, with heat. The heat is designed to enhance the chemotherapy's effectiveness by making cancer cells more susceptible to the drugs.
- BCG Instillation: Generally considered a first-line treatment for high-risk NMIBC.
- Chemohyperthermia: An alternative that uses chemotherapy with heat to enhance effectiveness.
- Recurrence-Free Interval: BCG showed a significantly better recurrence-free interval compared to chemohyperthermia.
- Progression-Free Interval: Both treatments showed similar results in preventing the cancer from progressing.
Making Informed Decisions About Bladder Cancer Treatment
The choice between BCG instillation and chemohyperthermia for bladder cancer treatment is complex. The study provides crucial insights for patients, their families, and healthcare providers, emphasizing the need for a tailored approach. As research continues, advancements in bladder cancer treatment will likely lead to even better outcomes. Always consult with a healthcare professional to discuss the best treatment plan based on your individual needs and the specifics of your condition.
