Battling the Bacteria: Understanding Deadly Infections in Urinary Tract Infections
"Unraveling the Risks and Saving Lives: A Deep Dive into Pseudomonas Aeruginosa and its Threat to Your Health"
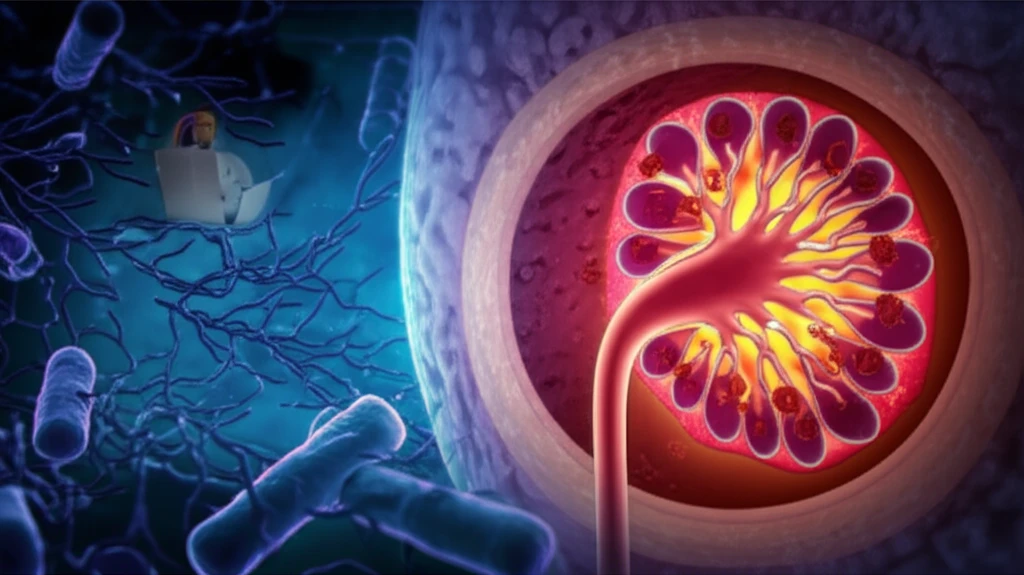
Urinary tract infections (UTIs) are a common nuisance, often easily treated with antibiotics. However, in some cases, these infections can escalate, leading to severe complications. One such complication is bacteremia, a bloodstream infection, particularly dangerous when caused by the bacterium Pseudomonas aeruginosa. This article delves into the complexities of P. aeruginosa infections in the context of UTIs, exploring the risk factors associated with mortality and offering insights into prevention and treatment.
Pseudomonas aeruginosa is a resilient and opportunistic pathogen, frequently found in various environments, including hospitals. When it infects the urinary tract, it can quickly spread to the bloodstream, leading to a condition called bacteremia. The severity of this infection can range from mild to life-threatening, underscoring the need for prompt diagnosis and effective management. Understanding the specific risk factors that contribute to mortality in these cases is crucial for improving patient outcomes.
This article draws from recent research to provide a comprehensive overview of P. aeruginosa bacteremia linked to UTIs. We will explore the clinical factors that increase the risk of death, discuss the importance of early intervention, and highlight preventive measures. This information is essential for both healthcare professionals and individuals seeking to understand and mitigate the dangers of this potentially deadly infection.
The Deadly Duo: Pseudomonas Aeruginosa and UTIs
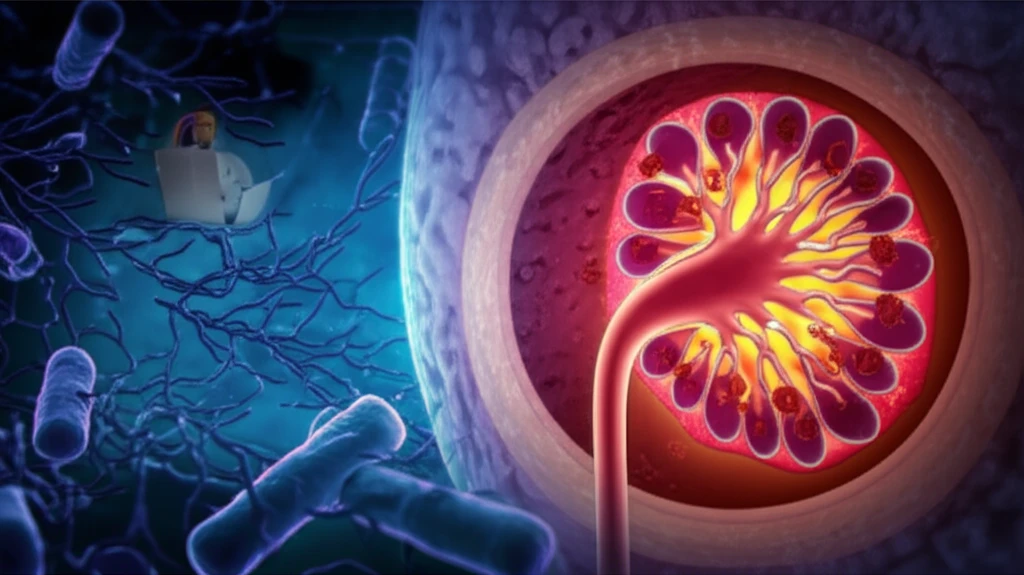
Pseudomonas aeruginosa is a bacterium that poses a significant threat, especially in healthcare settings. It's known for its ability to resist many antibiotics, making infections difficult to treat. When this bacterium enters the urinary tract, it can cause a UTI. If left unchecked or if the infection is particularly aggressive, the bacteria can invade the bloodstream, resulting in bacteremia. This is a serious condition requiring immediate medical attention.
- Weakened Immune Systems: Patients with compromised immune systems are less able to fight off the infection.
- Underlying Health Conditions: Diseases like diabetes and heart disease can increase susceptibility.
- Recent Medical Procedures: Invasive procedures can provide an entry point for bacteria.
- Antibiotic Resistance: The bacteria's resistance to antibiotics complicates treatment.
Empowering Prevention and Promoting Health
Understanding the risks associated with Pseudomonas aeruginosa bacteremia is the first step toward effective prevention and treatment. Early detection of UTIs, prompt medical attention, and adherence to prescribed treatments are crucial. For healthcare providers, awareness of the risk factors and the implementation of best practices in infection control are essential. By staying informed and taking proactive measures, we can collectively reduce the impact of this potentially deadly infection and safeguard public health.
